While most expectant mothers are excited, many are also anxious about giving birth, especially first-time mothers. Perineal trauma is something many expectant mums are fearful about.
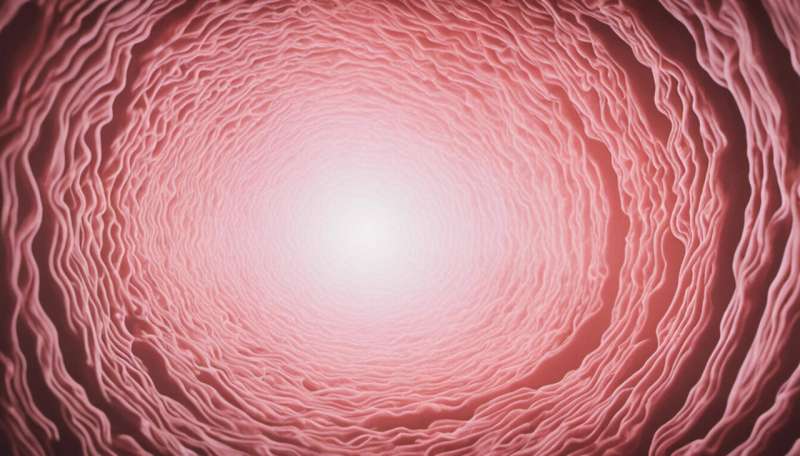
It is hard to comprehend being able to give birth to an entire human, but a woman’s vagina is pretty amazing, and nature has designed it to accommodate the baby. Hormones, increased blood supply and a clever, stretchy design all play a role in making this happen. No muscles in the female body are able to stretch without rupturing as much as those of the pelvic floor.
The perineum is the soft tissue between a woman’s vagina and anus, and it has the capacity to stretch significantly during birth. However, it can tear, or may be surgically cut if medically indicated and consented to by the woman (called an episiotomy).
When women have their first baby, they are more likely to have some perineal tearing. Most tears heal well and are never thought about again, but for some women there is ongoing pain and psychological trauma.
Perineal trauma prevalence
There are different degrees of perineal trauma (1st, 2nd, 3rd and 4th). First-degree (involves skin but not muscle) and second-degree tears (involves perineal muscles) are the most common. Third- and fourth-degree tears, known collectively as “severe perineal trauma” are more serious, as they also involve the anal area and can lead to long term consequences, such as pain and incontinence for women.
In Australia, the latest statistics show more than one in four women have no perineal tearing during the birth (more likely when not the first baby), 21% have a 1st degree tear, 30% have a 2nd degree tear and less than 3% have a 3rd or 4th degree tear (more common with the first baby).
Around 24% have an episiotomy, which is worrying as this has doubled in the past ten years (12% in 2009), and there is evidence the recovery is more painful than if the perineum tears naturally.
There is little doubt the rates of perineal trauma have increased over the past 100 years, with early midwife records indicating most women had no tearing.
An increase in the use of birthing interventions such as vacuum, forceps and episiotomy (which can cause further tearing), women giving birth at an older age to fewer babies, and greater vigilance by midwives and doctors when examining the perineum after birth have all played a role in the increased perineal trauma rates we see today.
Rates of perineal trauma vary across the country, with one report finding a 12-fold difference between hospitals, ranging from six per 1,000 births in some hospitals to 71 per 1,000 births in others.
This difference could come from varying hospital practices such as more frequent use of forceps and vacuum, or from the demographics of the women in a given area (more women having their first baby, or even the country of birth of the women).
How to reduce perineal tearing
There are recommendations on how to reduce the chance of perineal tearing and trauma, based in part on our research.
During pregnancy:
(1) perineal self-massage (or with help from your partner) after 34 weeks of pregnancy can help protect your perineum and reduce the risk of third- and fourth-degree perineal tears
(2) pelvic floor muscle training may help prepare you for labor and birth and reduce the possibility of a third- or fourth-degree perineal tear.
During a vaginal birth:
(3) applying warm compresses to the perineum during the second stage of labor (when pushing and giving birth) can significantly reduce the risk of a third or fourth degree perineal tear
(4) slowing the rate at which the baby’s head and shoulders emerge, with the help of your birth attendants, may help prevent perineal injuries
(5) perineal massage performed by your health-care professional during the second stage of labor may reduce the risk of third- and fourth-degree perineal tears. However, some women may not feel comfortable with this option, and it is not recommended for everyone
(6) listening carefully to your midwife’s voice and following their instructions can help the baby emerge from your vagina gently and slowly. For example, your midwife will tell you to breathe and not push just before your baby is born
(7) perineal trauma is less common when women give birth in home-like environments such as at home or in a birth center, where they have less medical intervention, can use water for pain relief and give birth in upright birth positions.
In a new paper we have also found having two midwives in the room in the late stage of birth, instead of one, can reduce perineal trauma by up to 31%. Our study found having a second midwife in the room meant one of them was focused on the woman at all times, and was not distracted by other things that needed to be done. It also meant they could give suggestions and reinforce the first midwife’s words to the mother during the birth.
Treatment and recovery
Following the birth, your midwife or doctor will stitch any perineal trauma that needs to be repaired in the birthing room, and these stitches dissolve over the coming weeks. Some tears are minor and do not require stitches.
Most perineal wounds heal well by resting, applying ice for the first day or two if swollen, changing sanitary pads and keeping the perineum clean, gentle pelvic floor exercises after a couple of days to help healing, and adequate pain relief.
After birth, if you have problems with your perineum, don’t just put up with it. Contact your midwife or doctor to get further advice.
Hannah Dahlen, Christine Rubertsson and Malin Edqvist, The Conversation

