Patients with cancers stemming from non-reproductive organs, such as bladder and liver cancer, have striking discrepancies in incidence, progression, response to treatment and survival outcomes depending on their sex. In almost all cases, male patients have worse prognoses and outcomes. This phenomenon has puzzled the scientific community for decades.
A study published today in Science Immunology and led by researchers in the Pelotonia Institute for Immuno-Oncology (PIIO) at The Ohio State University Comprehensive Cancer Center—Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC—James) examined the differences in intratumoral immune responses between male and female cancers of non-reproductive origin
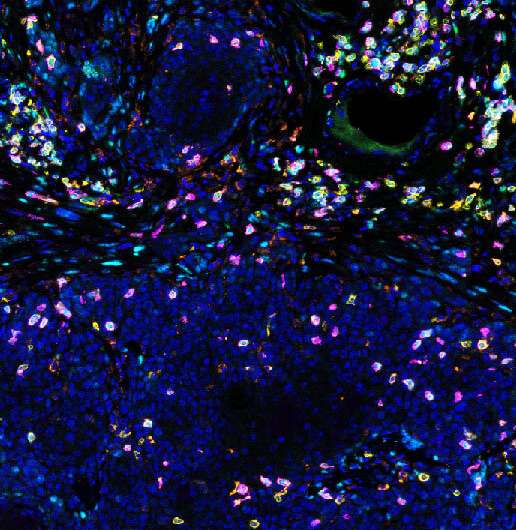
The focus of this research was the T cell immune response to malignancy, a key determinator of outcomes in cancer, and an important target that has contributed to the renaissance of cancer immunotherapy seen in recent years. The study reported a landmark finding that describes how male sex hormones contribute to cancer-related sex bias via the modulation of CD8+ T cells—a population of cells often referred to as cancer “killer” cells, which mediate adaptive immunity and are critical for mounting an anti-tumor response.
“Collectively, these findings highlight androgen-mediated promotion of CD8+ T cell dysfunction in cancer and suggest broader implications for therapeutic development to address sex disparities in health and disease,” said the study’s senior corresponding author Dr. Zihai Li, cancer immunologist, medical oncologist and founding director of the PIIO at OSUCCC—James.
Androgens are sex hormones more highly present in males. This study revealed that CD8+ T cells from cancers in male subjects, including human patients and mice, are more likely to have characteristics of a weakened anti-tumor immune function, also known as “exhausted” T cells. Androgen signaling promotes the progenitor exhausted CD8+ T cell phenotype via modulating expression of TCF1, a master regulator of CD8+ T cell function.
“Androgen-mediated promotion of CD8+ T cell dysfunction results in faster tumor growth and worsened outcomes, and targeting of this signaling cascade holds a crucial key to improving current cancer immunotherapies,” said Li, who is also a professor in the Ohio State College of Medicine.
Ohio State University Comprehensive Cancer Center

