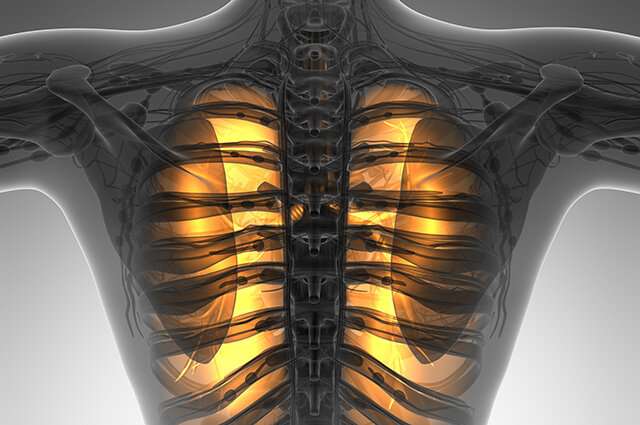
Take a deep breath in. Now, slowly, let it out. This simple activity is something we do all day long and seldom think about. But our lives depend on it. Every cell in the body needs oxygen, which is in the air we breathe.
Your lungs receive this oxygen and then move it into the bloodstream. Each cell in the body exchanges oxygen for carbon dioxide, a so-called “waste gas” that your bloodstream carries back to the lungs, where it is exhaled.
Even if you learned all of this in high school biology class, you likely haven’t thought a lot about your lungs—that is, until you’ve had reason to do so. COVID-19 had many of us focusing on our respiratory health, of course, but conditions like the common cold, seasonal allergies, and asthma also cause irritation to these highly sensitive organs.
And, while you are aware that smoking, pollution, and viruses can injure the lungs, you may not realize that obesity and stress can harm them, too.
“Lung health affects the health of all our other organs and organ systems, especially our brain, circulation, gut, immune function, and musculoskeletal system,” says Stephen Baldassarri, MD, MHS, a Yale Medicine pulmonary, critical care, and addiction medicine specialist. “Our lungs and airways are directly connected to the outside world. With every breath, we are inhaling what’s in our environment. And, ideally, we should only inhale clean air.”
We talked more with Dr. Baldassarri and other Yale Medicine specialists, from allergy and immunology to obesity medicine, about lung health.
How obesity affects your lungs
There’s a reason people who are overweight or obese easily get out of breath going up a flight of stairs or doing other physical activities.
“An important aspect of obesity is how it affects lung volume,” explains Jorge Moreno, MD, a Yale Medicine obesity medicine specialist. “If someone is obese, they can’t always get a full breath or full volume into their lungs, which can create breathing problems.”
Specifically, extra abdominal fat inhibits the ability of the diaphragm (a wall of muscle between the chest and abdomen) to properly draw in air and expand the lungs. People who are obese usually have smaller lung volume because of this, which leads to breathlessness, Dr. Moreno says.
There are also hormonal factors at play, for both men and women. As fat builds up under the skin, the fat cells secrete hormones. These hormones can cause inflammation throughout the body, including in the lungs, Dr. Moreno explains.
Severe lung inflammation was an early problem among many COVID-19 patients. It was no surprise to physicians, such as Dr. Moreno, that obesity emerged as a leading risk factor for severe illness from COVID-19.
“There are two stages to COVID. The first involves cold-like symptoms, which are typical and, in many cases, they resolve,” Dr. Moreno says. “The other is the inflammatory stage, in which the lungs can become inflamed and damaged, potentially leading to problems with the heart and other organs. This is what led to severe disease and death.”
Obesity is what Dr. Moreno calls “a pro-inflammatory state.” If you add the effects of the virus on top of it, the theory is that inflammation is increased even more, he adds.
Even for people who managed not to get sick with COVID, the pandemic presented challenges. For instance, working from home, being glued to a computer much of the day, and putting in more hours, can make it difficult to find time to eat well and exercise.
“One piece of advice is to try and plan meals better. We can be flexible if we are at home, but that might mean grazing on whatever is in the fridge,” suggests Dr. Moreno. “Instead, try to be mindful of what you are eating. This goes for alcohol, too.”
Dr. Baldassarri recommends daily exercise and a diet consisting mainly of whole foods, vegetables, fruits, high fiber, and plant-based protein. “Try to engage in moderate-to-vigorous exercise at least 20 minutes every day,” he says. “If you can do more than that, it’s even better. But any amount of exercise, even a few minutes per day, is better than none. A healthy diet and exercise are great for lung-specific and overall health.”
How stress harms the lungs
In stressful situations, your body releases hormones, such as adrenaline and cortisol, that can contribute to rapid breathing. If your lungs are healthy, this is not dangerous. However, in people with chronic lung conditions, such as COPD (chronic obstructive pulmonary disease) or asthma, the lungs can’t move as much air in and out as they should. This can increase shortness of breath and can contribute to a sensation of panic.
More cortisol release can also cause other challenges, including increased appetite. Or, for those who smoke, stress can cause cravings to smoke more, notes Dr. Baldassarri.
“We know that cigarette and alcohol sales increased during the pandemic,” Dr. Baldassarri says. “Those trends likely reflect the stress we have been feeling. Stress influences our entire body and is such an important determinant of our health.”
The best thing for lung health is to practice a healthy lifestyle, which includes eating well, exercising, not smoking or vaping, and reducing stress as much as possible, Dr. Baldassarri says. “We can reduce our stress by getting enough sleep at night and taking some time each day to do meditation and focused breathing exercises,” he says. “It’s also important to spend time with friends and family who bring us positive energy.”
How air quality impacts your lungs
Both indoor and outdoor pollutants can cause or worsen lung infections, cancers, and other conditions, including asthma.
In the home and workplace, chemicals, radon, asbestos, building and paint products, carbon monoxide, carpets (which can trap pollutants and allergens such as dust mites, pet dander, and mold), lead, and water damage are some examples of things that can make the air around us unhealthy.
Your exposure to outdoor air pollutants—from car exhaust to power plants to forest fires—can be harder to control, but it’s important to know that such exposures can also trigger asthma episodes, make people sick, and negatively affect how children’s lungs develop.
You can check your local air quality index, a system that tracks ozone (smog) and particle pollution (from ash, power plants and factories, vehicle exhaust, soil dust, and pollen) and other widespread pollutants, in order to know when to avoid spending too much time outside. The index is color-coded and ranges from “good” air quality in green to “very unhealthy” in purple.
Lots of media outlets, including websites, newspapers, TV, and radio stations, report the local air quality index, and you can also look up your location on airnow.gov. It’s especially important to avoid exercising outdoors in unhealthy air because the effects of pollution on the body are worsened by the deep, quick breaths people take during physical exertion. It’s also best to avoid exercising near high-traffic areas in general, and particularly when the air quality is poor.
People with asthma are especially sensitive to poor air quality, says Jason Kwah, MD, a Yale Medicine allergist and immunologist. “We know that asthma is more prevalent in urban areas and in people who live near major roadways,” he says.
How infections injure your lungs
Infectious respiratory diseases, including flu, COVID-19, pneumonia, pertussis (whooping cough), RSV, and the common cold can harm the lungs. This is especially problematic because these conditions spread easily from person to person.
Most types of lung infections can be treated, but they can also be dangerous for infants, seniors, and people who have a lung disease or a weakened immune system. Fortunately, there are vaccinations (with the exception of RSV and the common cold) available for many common diseases that affect the lungs.
One silver lining of the COVID-19 pandemic is how it has highlighted the importance of vaccination in general, says Geoffrey Chupp, MD, director of the Yale Center for Asthma and Airway Disease.
“Because of COVID, we have increased awareness about lung viruses—how they can affect the lungs, and the role vaccination plays in preventing these diseases,” he says. “Vaccination has been at the forefront of many people’s dinner table conversations, which is good. Public awareness is going to ultimately help people be better about taking care of their lungs.”
Carrie MacMillan, Yale University