A group of researchers at Children’s Hospital of Philadelphia (CHOP), in collaboration with Beam Therapeutics, have tested and developed an “off-the-shelf” chimeric antigen receptor T-cell (CART) using base editing, which is designed to allow for precise editing of the CART with less risk of unwanted and unforeseen outcomes that may accompany other editing methods. The CART, known as 7CAR8 and recently described in a paper in the journal Blood, is highly active against T-cell acute lymphoblastic leukemia (T-ALL) in multiple preclinical models. In the setting of relapsed or refractory disease, T-ALL often does not respond to chemotherapy and chance of cure is low. The hope is 7CAR8 will be an effective and life-saving therapy for these patients, if approved.
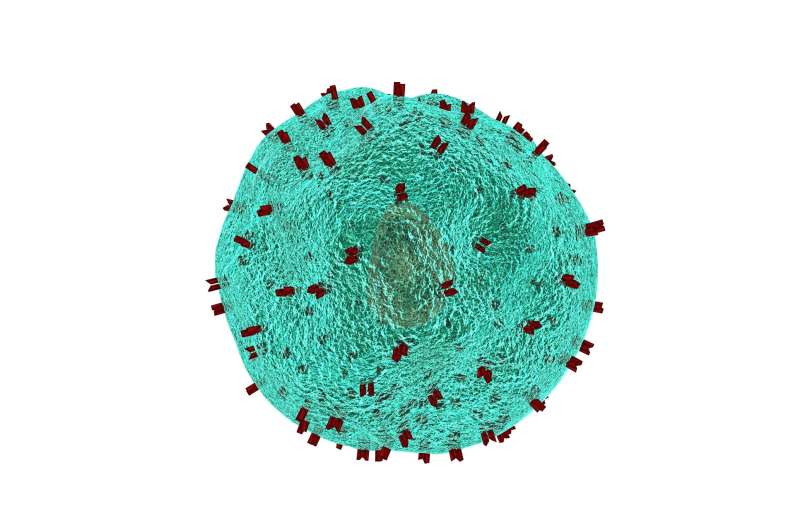
CAR T-cell therapy has revolutionized the treatment of relapsed or refractory blood cancers, with several products authorized by the Food and Drug Administration (FDA). However, those products involve harvesting and modifying T cells from patients with cancer, which comes with many challenges. A CART created from healthy donors would bypass many of those issues and could potentially provide an on-demand, “off-the-shelf” product. Such a product would require modifications to prevent graft-versus-host-disease (GVHD) and CART rejection by the patient’s immune cells.
To address these barriers, researchers have modified allogeneic CART products using genome-editing, but many of these tools—such as CRISPR-Cas9—rely on DNA double-stranded breaks (DSBs), which can cause unintended outcomes with potentially unforeseen consequences. These undesirable outcomes have substantial clinical implications and would potentially imperil the approval or utility of an “off-the-shelf” CART produced in this way.
Base editing is an emerging technology capable of making single base pair changes at specific points with high precision and efficiency. Base editors are designed for silencing gene expression without creating DSBs, potentially reducing undesired editing outcomes as compared to a technology like CRISPR-Cas9.
To determine if base editing to produce CART is clinically feasible, the CHOP researchers, led by Caroline Diorio, MD, an attending physician in the Cancer Center and in collaboration with Beam Therapeutics, tested an “off-the-shelf” CART for relapsed or refractory T-ALL, targeting the surface receptor CD7, which is highly expressed on the vast majority of T-ALL blasts. Given that CD7 is also expressed on the surface of healthy cells, the researchers used cytosine base editing to make four base edits to create 7CAR8, which is believed to be the first CAR T product with four simultaneous genetic edits progressing towards clinical development.
In multiple in vivo and in vitro preclinical studies, the researchers observed that 7CAR8 did not impact T-cell proliferation or cause genomic rearrangement products. They also observed that 7CAR8 was highly active in vitro and in vivo in a cell line model and in multiple patient-derived xenograft (PDX) models of T-ALL. Sarah K. Tasian, MD, an attending physician and co-author on the study is currently testing this therapy in the lab in preclinical models of another pediatric cancer, acute myeloid leukemia (AML).
“Studies in the laboratory suggest 7CAR8 is highly active in preclinical models and could potentially be a curative therapy for children and adults with relapsed or refractory T-ALL, if approved. It also has potential for use as a treatment for other CD7+ malignancies such as T-cell lymphoblastic lymphoma and subsets of acute myeloid leukemia,” said senior study author David T. Teachey, MD, an attending physician and Director of Clinical Research at the Center for Childhood Cancer Research at CHOP. “Based on these results, we plan to translate 7CAR8 into the clinic for children and adults with relapsed or refractory T-ALL. This highly adaptable editing approach also has the potential for use to create ‘off-the-shelf’ CARs for other immunotherapy targets.”
Jennifer Lee, Children’s Hospital of Philadelphia

