Chronically stressful conditions of daily life such as racism, pollution and poverty have a direct impact on the cellular mechanisms that drive lethal, invasive forms of breast cancer, according to a study led by Duke Cancer Institute researchers.
Publishing June 13 in the journal npj Breast Cancer, the findings provide insight into one of the most pervasive health disparities between White and Black people. Among aggressive subtypes like triple negative and inflammatory breast cancers, Black women have higher incidences and lower survival rates than White women.
“When talking about breast cancer, these disparities are not just in the U.S., but are global,” said senior author Gayathri Devi, Ph.D. associate professor in Duke’s departments of Surgery and Pathology and program director of the Duke Consortium for Inflammatory Breast Cancer at Duke Cancer Institute. “There is a complex interplay among societal stress factors—access to care, racism, pollution, and the many problems associated with poverty—and the impact these stresses impose at the molecular level inside the body.
“Among people of African ancestry, exposures to these stress factors have spanned generations and geographies and have resulted in population- and individual-level differences in physiology, genetics and genomics,” Devi said.
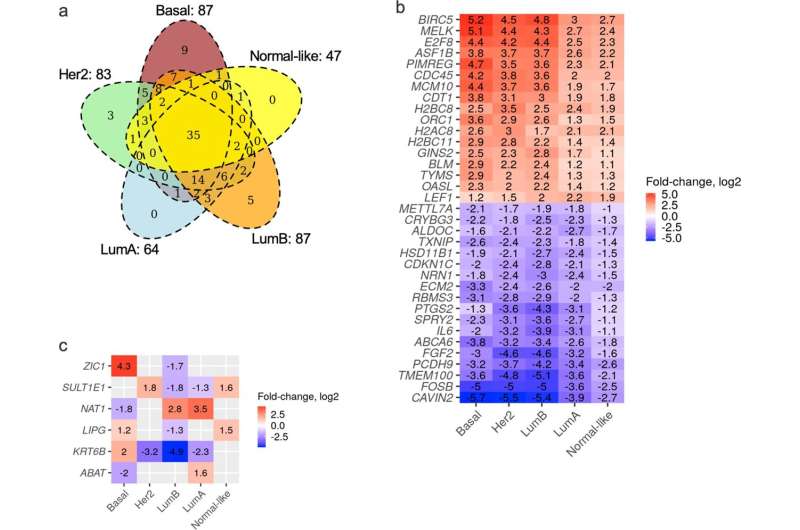
Devi and colleagues, using The Cancer Genome Atlas, identified specific genes from a set of 226 genetic patterns of adaptive stress response that differ depending on the breast cancer subtype. These stress response genes play functional roles in cancer development, including cell life cycles, DNA damage response, signaling pathways, and regulation of cell death-related processes.
“Previous studies from our lab and others show that tumor cells respond to cellular stress differently than normal cells,” Devi said. “When normal cells see stress, they pause protein synthesis and repair any gene changes. If they are unable to make repairs, they begin the process of cell death.
“With chronic stress, tissues and cells in the body react differently and adapt,” Devi said. “This study explored that process. There’s a term called allostatic load, and that describes a cumulative burden of chronic stress and life events that occurs in individuals and even in populations of people.”
Under chronic stress conditions, tumor cells adapt to develop a high tolerance for stress, avoiding the normal cell death process and continuing to proliferate. Twenty-nine of these stress response genes exhibited race-related differences in their activation.
The study also associated gene sets known to be involved in cancer signaling and response to oxidative stress with worse breast cancer patient survival outcomes.
Because Black patients’ breast tumors exhibit higher oxidative stress markers compared to White patients, the findings highlight the importance of understanding the underlying biology of aggressive breast cancer subtypes as part of the diagnosis and treatment process, Devi said.
“Where race- and/or ancestry-related disparities exist in incidence, treatment, and survival outcomes, identifying the tumor biology has the potential to aid in development of new biomarkers and treatment strategies to mitigate these disparities,” Devi said.
Sarah Avery, Duke University

