A new Yale study has found that the liver plays a major role in regulating feeding behavior in mice, a discovery that could have implications for people with eating disorders and metabolic diseases. The study, which was done in collaboration with colleagues in Germany, also adds to a growing body of evidence that shows the most advanced part of the brain, the cerebral cortex, is affected by the rest of the body, not just the other way around.
“One takeaway of this work is that the classical way of trying to understand brain functions by only looking at the brain itself is not giving you the full picture,” said Tamas Horvath, the Jean and David W. Wallace Professor of Comparative Medicine at Yale School of Medicine and a senior author of the study published June 27 in Nature Metabolism.
In a series of experiments, the research team uncovered a circuit by which the brain and liver communicate with—and control—each other. The two key participants of this conversation are a group of cells known as agouti-related protein (AgRP) neurons, which are found in the hypothalamus region of the brain, and a type of lipid secreted by the liver called lysophosphatidyl choline (LPC).
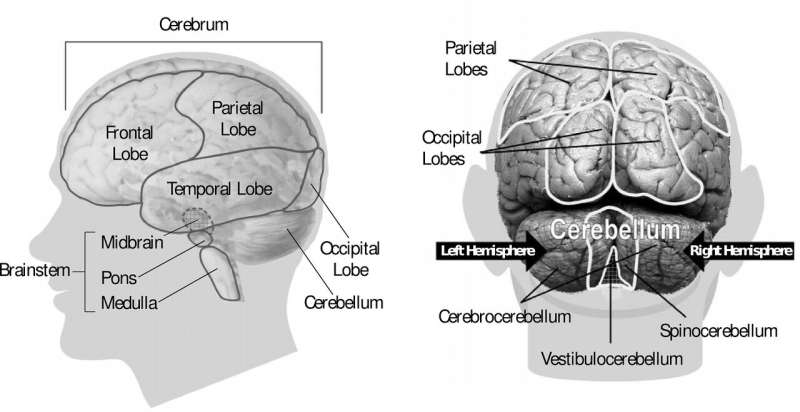
AgRP neurons, which communicate with the cerebral cortex, the outer layer of the brain associated with complex behaviors and abilities, are essential for promoting feelings of hunger. But they also communicate with other parts of the body, like the liver and pancreas; when humans are hungry, these neurons play a critical role in releasing lipids from fat stores in the body.
Once LPC is secreted by the liver, an enzyme in the blood quickly converts it to lysophosphatidic acid, or LPA. Other researchers have shown that LPA can alter neuronal activity in the brain.
In this study, the researchers observed that after fasting, mice had higher levels of LPA in both the blood and the cerebrospinal fluid, the special liquid found within the central nervous system. This rise in LPA levels caused an increase in neuronal activity in the cortex, which triggered a heightened post-fasting appetite. And all of these effects were dependent on AgRP neuron function.
These findings suggest a circuit wherein AgRP neurons regulate the liver and lipid release and in which those lipids cycle back to the brain where they affect the cortex and its functions.
Horvath says more research is needed to determine if a similar circuit exists in humans, but he and his colleagues did find some evidence that it might. Mice that experience a mutation leading to greater LPA-induced neuronal activity eat more and weigh more than their typical mouse counterparts. Humans with this same genetic mutation tend to have higher body mass indexes and a greater prevalence of Type 2 diabetes than people without the mutation.
“We still need to more rigorously explore whether these mechanisms are relevant for humans, but if they are then we can start to investigate whether we can exploit the mechanisms in order to treat eating disorders and other conditions,” said Horvath. “But this shows the liver can be a major driver of behavior. And it adds to the argument that staying in the brain to understand the brain is not sufficient.”
Other Yale authors on the study are Bernardo Stutz, Zhong-Wu Liu, and Matija Sestan-Pesa.
Mallory Locklear, Yale University

