A new study finds that signs of covert consciousness—subtle brainwaves detectable with EEG—are the strongest predictor of eventual recovery for brain-injured patients who otherwise appear completely unresponsive.
The findings suggest brainwave analysis has the potential to completely change how unresponsive patients with acute brain injury are managed.
The study was published online in Lancet Neurology.
“One of the most difficult challenges in ICU care is determining whether an unresponsive patient with a brain injury is likely to recover and to identify those that may benefit most from rehabilitation,” says study leader Jan Claassen, MD, associate professor of neurology and chief of critical care and hospitalist neurology at Columbia University Vagelos College of Physicians and Surgeons.
Standard bedside assessments alone do not always predict clinical outcomes. In the intensive care unit, doctors routinely assess the prognosis of brain-injured patients by asking them to respond to a simple verbal command, such as “move your hand” or “stick out your tongue.” Those who do not respond to these commands are thought to be unconscious. In the absence of any other explanations for this unresponsiveness, injuries may be considered so severe that patients are unlikely to regain consciousness.
“But in some rare cases, unresponsive patients do eventually regain consciousness and may make meaningful progress toward recovering many day-to-day functions many months later,” says Claassen, who also is an associate attending neurologist at NewYork-Presbyterian/Columbia University Irving Medical Center. “We just don’t have a reliable way to predict who those patients are.”
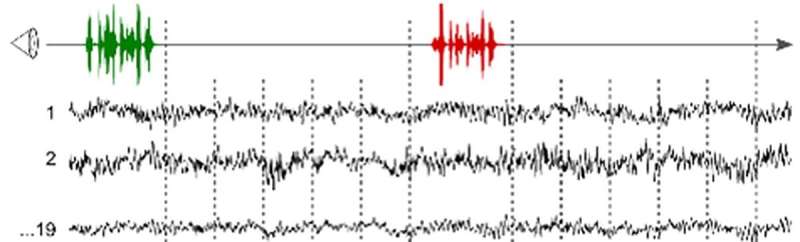
In a previous study, Claassen and colleagues found that while many brain-injured patients cannot physically respond to verbal commands, a few of them generate brainwave activity in response to those commands, suggesting they have some level of consciousness.
“We found that covert consciousness is an independent predictor of recovery, stronger than any other established factor we looked at, including the patient’s age, initial Glasgow Coma Scale score (a standard measure of the extent of neurological injury), or the cause of the brain injury,” Claassen says. “In the future, cognitive-motor dissociation may be another factor to consider when assessing a patient’s prognosis.”
Currently, only a few select centers are using EEG to study covert consciousness, and a significant amount of biomedical expertise is required to look for it. Claassen’s team is working to refine the artificial intelligence software and approach so that EEG could be used in ICUs everywhere to diagnose covert consciousness.
The researchers are investigating the underlying mechanisms of covert consciousness to better understand why a patient who has brainwave activity in response to different motor commands and is not paralyzed cannot physically act on these commands. They also are interested in studying how degrees of covert consciousness are linked to clinical outcomes.
This state is called cognitive-motor dissociation, or covert consciousness, and can be picked up with customized artificial intelligence software applied to standard EEG signals recorded while patients listen to motor commands. (This machine learning algorithm was made freely available by the investigators with their earlier publication.)
The previous study found that patients with covert consciousness were more likely to recover, but the study was too small to determine how useful EEG, together with other known predictors, may be in predicting patient outcomes.
In the new study, involving a larger group of patients, the researchers asked whether the presence of covert consciousness can reliably predict which patients will have a meaningful recovery over the next 12 months. Of 193 patients, covert consciousness was detected in 27 (14%). Those with covert consciousness had consistently higher and faster rates of recovery than those without covert consciousness. Within one year, 41% of patients with covert consciousness made a full recovery, compared with 10% of patients without covert consciousness. Most of the patients with covert consciousness began to improve at three months, whereas patients without covert consciousness who recovered took much longer to show signs of improvement.
Columbia University Irving Medical Center

