Lifestyle changes and medication are more effective in combating the risk of stroke than invasive procedures, a Monash University study shows.
A Monash researcher has analyzed more than four decades of data relating to common treatments for advanced carotid artery stenosis, one of the leading causes of stroke, and found surgery and stents have very limited impact, if any, in preventing stroke.
Carotid artery stenosis is a disease caused by the build-up of fatty deposits (plaques) in the main artery that delivers blood to the brain. The disease affects one in 10 people by age 80 and it is a major cause of stroke—the third-biggest cause of death, occurring when blood supply to the brain is restricted.
The Monash analysis, published in the open science journal Frontiers in Neurology, found that lifestyle factors—such as diet, exercise and quitting smoking—had a significant impact in reducing stroke risk when combined with appropriate medication.
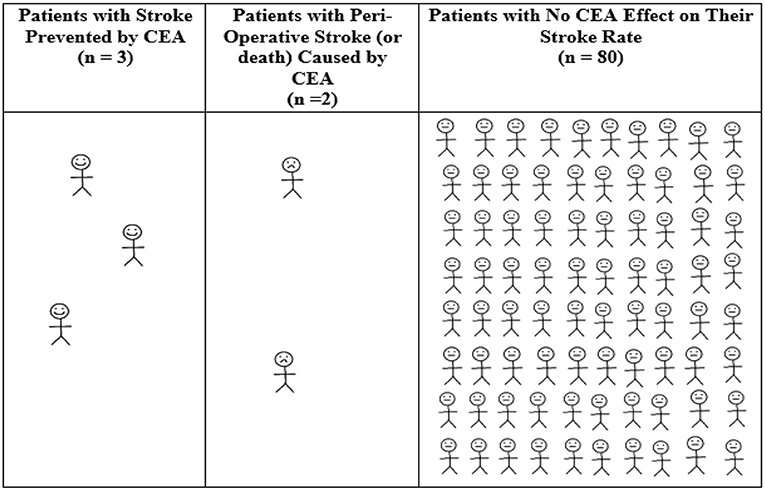
The stroke risk in symptom-free patients with advanced carotid stenosis fell by at least 65 percent to 1 percent or less in those using non-invasive measures alone, the study showed. This is similar to, or lower than, the stroke rate in patients who underwent carotid surgery or stenting in past trials.
Study author Associate Professor Anne Abbott from Monash’s Central Clinical School, said the findings dispel a common misconception that surgery or stenting is the best treatment for carotid artery stenosis, when the procedures often cause more harm than good.
“This is a widespread furphy that leads to inappropriate patient care, causing large-scale harm and premature death, while wasting vital health resources,” Associate Professor Abbott said.
“People need to understand that they have the greatest power to prevent their own stroke. Healthy life habits, including physical activity, diet and quitting smoking, combined with appropriate medication, help mitigate major risk factors such as high blood pressure and cholesterol, and very effectively reduce the risk of stroke and heart attack.”
There are currently four types of intervention used to reduce stroke risk in carotid stenosis patients: carotid surgery (endarterectomy), carotid stenting, a new hybrid procedure known as trans-carotid arterial revascularization (TCAR), and medical (non-invasive) intervention with lifestyle coaching and medication.
“Stroke rates are now so low with non-invasive intervention alone that carotid artery procedures are unlikely to provide benefit to the vast majority of patients and have no current proven benefit for any patient,” Professor Abbott said. “Yet carotid artery procedures are still very commonly done in Australia and overseas and they continue to cause significant complications, including stroke, death and heart attack, and they are costly.”
Professor Abbott is calling on the health sector to incorporate best practice non-invasive interventions and stop unnecessary procedures in order to deliver the best outcomes for their patients.
Monash University

