Two new treatments for Crohn’s disease showed roughly equal performance in a clinical trial, according to findings published in The Lancet.
This allows clinicians and patients to make treatment choices based on tolerance, according to Stephen Hanauer, MD, the Clifford Joseph Barborka Professor and a co-author of the study.
“The safety and efficacy of two agents with different mechanisms of action appears to be quite comparable over one year,” said Hanauer, who is also a professor of Medicine in the Division of Gastroenterology and Hepatology.
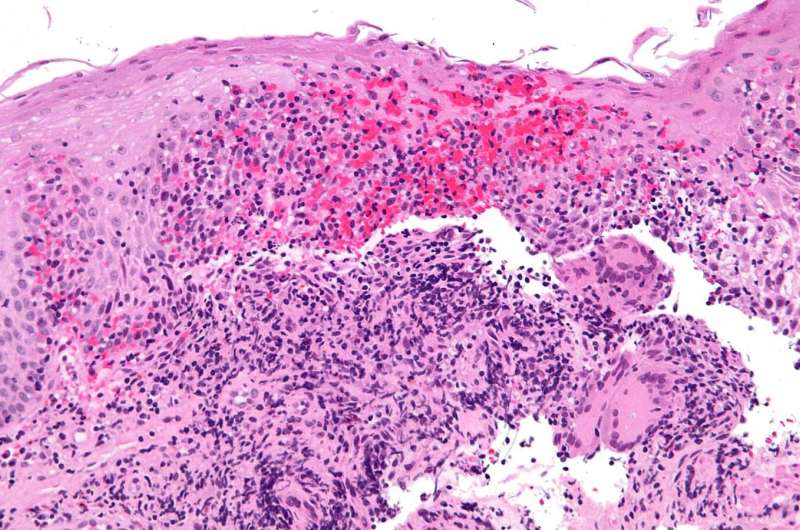
Crohn’s disease (CD) is a chronic, progressive inflammatory bowel disease, causing abdominal pain, weight loss and fatigue. Treatment for CD has typically focused on alleviating symptoms to achieve clinical remission using corticosteroids or immunomodulators, but a need for more effective treatment remains, Hanauer said.
“While there are numerous therapies and mechanisms of action for drugs approved for moderate-severe Crohn’s disease there has been a therapeutic ceiling as far as outcomes are concerned, with usually less than 50% of patients in long-term remission,” Hanauer said.
Recently, several biologic agents have been approved for use. Adalimumab is a monoclonal antibody that reduces inflammatory cytokines by inhibiting tumor necrosis factor alpha. Ustekinumab is another monoclonal antibody, though the drug targets a different set of proteins: interleukin 12 and interleukin 23.
In the study, investigators recruited nearly 400 patients with Crohn’s disease and randomly assigned them to receive ustekinumab or adalimumab. Patients reaching clinical remission were similar between both groups: 124 (65%) of 191 patients in the ustekinumab group versus 119 (61%) of 195 in the adalimumab group. No deaths occurred through one year of study, though slightly more patients in the ustekinumab group discontinued study treatment before one year had elapsed. Further, patient-reported measures of disease severity decreased similarly over the course of the study.
Both treatment regimens resulted in clinical remission with similar toxicity profiles. The findings should inform provider and patient decisions in therapy selection, Hanauer said.
“There are numerous options for patients with moderate-severe disease. However, the key is to treat patients with an effective regimen and treat to targets as early in the course as possible since we do not have any drugs that impact on fibrosis once it occurs,” Hanauer said.
Will Doss, Northwestern University

