Dr. Yuanjie Mao has led a study published in JAMA Oncology looking at the correlation between daily insulin dose and cancer incidence (the number of new cases) among patients with type 1 diabetes, finding that higher insulin dose is positively associated with cancer incidence and that the association is stronger among those with insulin resistance.
“In patients with type 1 diabetes, our results show that traditional metabolic factors such as obesity (represented by body mass index), sugar control (represented by Hemoglobin A1c), and blood pressure control do not associate with cancer incidence,” Mao said. “However, cancer incidence was higher for those who took larger dose of insulin. Our results implied that clinicians might need to balance the potential cancer risk when treating patients with type 1 diabetes on a high daily insulin dose or that improving insulin sensitivity may be preferred than simply increasing the insulin dose.”
To conduct the study, Mao collaborated with Wenjun Zhong, Ph.D., an epidemiologist of Merck Research Labs in West Point, Pa. to analyze the associations of more than 50 common risk factors such as smoking, alcohol use, exercise, metabolic risk factors, medication use and family history with cancer incidence in 1,303 patients with type 1 diabetes whose data were collected over 28 years. They acquired data from The Diabetes Control and Complications Trial (DCCT) and its follow up, the Epidemiology of Diabetes Interventions and Complications (EDIC) study, from the National Institute of Diabetes and Digestive and Kidney Diseases Central Repository and performed statistical analysis on them. DCCT was a controlled clinical trial originating with 1,441 patients with type 1 diabetes who were randomized into conventional diabetes therapy or intensive therapy to assess whether reducing hyperglycemia would decrease the risk of complications of type 1 diabetes.
Mao also found that age and sex are associated with cancer incidence when evaluated separately and that a daily insulin dose posed a higher risk of cancer than age, especially a higher insulin dose.
According to the paper, when the daily insulin dose is classified into three groups, low: less than 0.5; medium: greater than or equal to 0.5 or lower than 0.8; and high: greater than or equal to 0.8 units/kg per day, the hazard ratios were significantly higher in the high dose versus the low dose group. Cancer incidence was 2.11, 2.87, and 2.91 per 1,000 persons in the low, medium, and high insulin dose groups, respectively.
He went on to explain that specifically, women carry a higher risk than men; however, it was unclear what risk factors may contribute to the higher cancer incidence in type 1 diabetes.
“We know that people with type 1 diabetes have a higher incidence of cancer compared to people without diabetes,” Liz Beverly, Ph.D. co-director of the diabetes institute and professor in the Heritage College, said. “Dr. Mao’s research identifies a potential mechanism to explain this association. His findings will lead to continued research in this area and potential policy changes in cancer screening and insulin dosing recommendations.”
Although previous studies have concluded that patients with diabetes have a higher risk of cancer in general, this is the first study to explore the associated cancer incidence factors in type 1 diabetes.
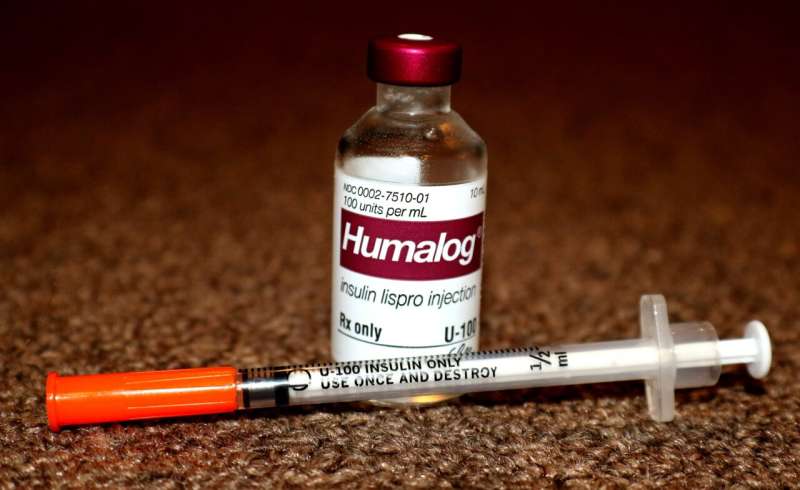
“Type 1 diabetes accounts for an estimated five to 10 percent of all diabetes cases, and recent studies in type 1 diabetes also found a higher incidence of certain cancers such as stomach, liver, pancreas, endometrium and kidney cancers in the population compared with the general population,” Mao explained. “Whereas, in type 2 diabetes, increased risk is attributed to metabolic factors such as obesity, chronic inflammation status, and insulin resistance.”
Although the results of the study suggest that the higher the dose of insulin, the higher the cancer incidence, Mao says further investigation is still necessary.
Mao graduated from Peking University with an M.D. and Ph.D. and had residency training in internal medicine at the Cleveland Clinic Akron General and fellow training in Endocrinology, Diabetes, and Metabolism at the University of Arkansas. Since then, he has been working at Ohio University as an assistant clinical professor in the Department of Specialty Medicine and the Diabetes Institute. He is also working with OhioHealth as an endocrinologist in the Castrop Center and at O’Bleness Hospital. His specialization is in diabetes, thyroid diseases, osteoporosis, and other endocrine disorders. In addition to the current study, he is also working on several other clinical trials on obesity, type 1 diabetes, and type 2 diabetes.
Ohio University

