A new biosensor capable of accurately monitoring the condition of a chronic wound has been developed by a team at Nottingham Trent University and Nottingham University Hospitals NHS Trust.
Wounds represent a burgeoning health care issue affecting thousands of patients in all health and social care settings, leading to a spiraling expenditure on an already overloaded health system.
One of the most urgent needs in wound management is the development of systems that allow clinicians to identify the early progression or deterioration of wounds.
The team of engineers and clinical academics at NTU and NUH says the aim is for the technology to be embedded into dressings so that they do not need to be continually removed and replaced to assess how a wound is healing.
They say that in time the technology—a textile-based printed protein sensor—could help to reduce the risk of patients becoming seriously ill, prevent amputation, and save time and money.
Patients can not currently assess the condition of a wound and health professionals are required to remove the dressing to assess it visually.
This can take time as patients require an appointment and removing the dressing too soon risks lengthening the healing process, making scarring worse, or introducing an infection. The dressing also needs replacing each time the wound is checked, which takes more time.
Chronic wounds include wounds as a result of serious injury or trauma, ulcers, pressure sores or through diseases such as diabetes.
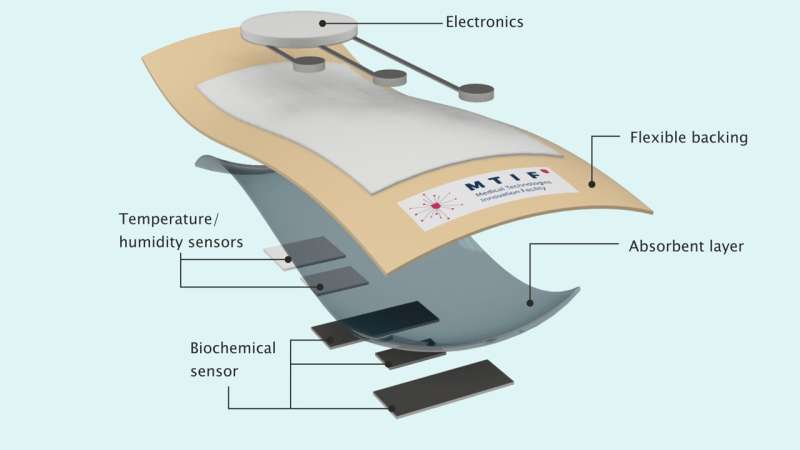
The new sensor—which is printed onto fabric—would be integrated in the dressing, uses electrodes to analyze the concentration of specific proteins in a wound constantly and in real time.
Using app-based technology, the patient would be able to take a reading and receive some simple information by holding a smartphone near to the dressing. They would then be able to book an appointment, if necessary, so that it can be checked by a clinician.
The miniature sensor, which is lightweight and flexible, would be able to determine whether the dressing required changing, can come off completely or if the wound has an infection.
The cost of treating wounds is thought to account for about least three percent of the total healthcare expenditure in most developed countries and since 2018 it is estimated that the UK is managing about 3.8 million patients with a wound in a clinical setting annually.
It was also estimated that health services in 2012 spent more than £5 billion (approximately USD$6 billion) on costs associated with wound care management.
The researchers say that now the technology is established, the next step will be to work with consultant clinicians and digital technology providers to look at moving it into commercial products.
The project also involves industry partner Kymira.
“There is currently no way to monitor the condition of a wound without booking an appointment, having the dressing removed and taking a look,” said researcher Dr. Yang Wei, an expert in electronic textiles and electronic engineering in Nottingham Trent University’s School of Science and Technology.
He says that “the sensor analyzes chemical biomarkers to give an indication of whether a wound is healing or not and could help remove a range of risks associated with continuous and laborious removal and replacement of dressings. As well as improving patients’ quality of life, it could speed up the healing process, help to avoid infection and avoid worsening scars by removing dressings while they are still forming.”
“Wounds can take months to heal and this could potentially be of great benefit to many people. It enables patients to monitor the wound themselves and reducing worrying about their condition in addition to saving time and money in the process.”
“It would also be consistent and quantifiable and help to remove the subjective nature of assessing a wound.”
Professor John Hunt of NTU’s Medical Technologies Innovation Facility, who was also involved in the study, said, “This research addresses a clear need for improved treatments. The approach will not only deliver on improved wound healing, it will reduce patient worries, reduce visits either at home or with the healthcare provider and enable people to manage their health and maintain greater independence.”
“We are delighted to be facilitating this research in MTIF as digital health solutions are a key part of the world delivering on future health needs.”
Professor Christine Moffatt CBE, who is professor of skin integrity at NUH, described these developments as having a massive potential to change the lives of thousands of people suffering with wounds and improve the delivery of effective care.
The Nottingham Trent University team’s work is published in Scientific Reports.
Nottingham Trent University

