A study led by researchers at the University of Oklahoma shows a connection between symptomatic COVID-19 infections and the ability of the central nervous system to respond to painful stimuli.
Christopher D. Black, Ph.D., associate professor in the Department of Health and Exercise Science, Dodge Family College of Arts and Sciences at OU, led the study with a doctoral student in his lab, Jessica A. Peterson. Peterson, the first author of the study, is now a postdoctoral researcher at the Pain Research and Intervention Center of Excellence at the University of Florida, Gainesville.
In late 2020, the scientific community began wondering what the potential long-term effects of COVID-19 infections might be. One of the common symptoms of COVID-19 infection is system-wide inflammation, which can lead to headaches and general aches and pains, also called myalgia.
“When you get inflammation, things that weren’t painful before now become painful,” Black said. “We realized we have all of these people who have had COVID-19, and there’s a chance they may be at a higher risk of developing chronic pain conditions when they get older. We wanted to see whether people who had experienced a COVID infection—even though they no longer have symptoms—if they have normal function in their central nervous system in relation to their ability to ‘correctly’ respond to a painful stimuli.”
The study, conducted from January through March 2021, included 59 participants separated into three groups. The symptomatic group included those who had previous symptomatic COVID-19 infections that were confirmed through PCR or antibody testing. An unexpected addition to the study became the asymptomatic group—those who had not known they had previously been infected by COVID-19 and had not experienced symptoms but were confirmed through antibody testing. The control group had neither experienced COVID-19 infection nor had antibodies present at the time of testing.
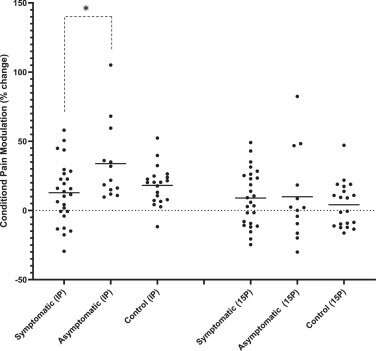
The researchers measured each person’s pain threshold—the amount of pressure applied to a muscle, in this case in the participant’s arm or leg, that it takes for the participant to report feeling pain. Second, the researchers measured pain modulation, or the signals sent from the central nervous system to the brain and spinal cord that can “change the volume” on how much pain a person reports.
To measure the pain modulation experienced by the test groups, the researchers followed the muscle pressure test with one of two experiments, a bout of knee extension exercise or a “cold presser test” where participants were asked to put their foot in a bucket of ice water for a brief period.
“These two tests, especially the ice water test (also called a conditioned pain modulation test), are used in clinical settings to help identify individuals who have or may be at a risk of developing a chronic pain condition,” Black said. “So, we measured each person’s pain threshold on their leg and on their arm. Then they would either do a bout of exercise with their leg and then we retest their pain threshold on the leg and the arm, or they would put their foot in the bucket of ice water and then we retest the leg and the arm. A ‘normal’ modulation response would result in an increase in their pain threshold—it would require greater pressure to be applied for them to tell us it hurt. However, in our symptomatic COVID participants, their pain thresholds did not change, indicating impaired conditioned pain modulation. Other studies have shown clear relationships between impaired pain modulation and the development of chronic pain conditions.”
The study’s finding shows a connection between participants who had experienced symptomatic, verified COVID-19 infections and the ability of their central nervous system to respond normally to a conditioned pain modulation test.
“As far as we can tell, these are some of the first data on the effects of COVID-19 on pain outcomes,” Black said. “We (in the U.S.) spend hundreds of billions of dollars on the treatment of chronic pain conditions every year. It’s one of the leading causes of adult disability. Chronic pain is already a huge, chronic burden on the health care system, and we now have hundreds of millions of people in the U.S. who have had a COVID infection. The interaction of COVID and pain need to be further studied because if there is a chance of lasting impairments in pain modulation, this may put individuals at a greater risk in the future of developing a chronic pain condition.”
The study was published July 21, 2022, in the Journal of Pain.
University of Oklahoma

