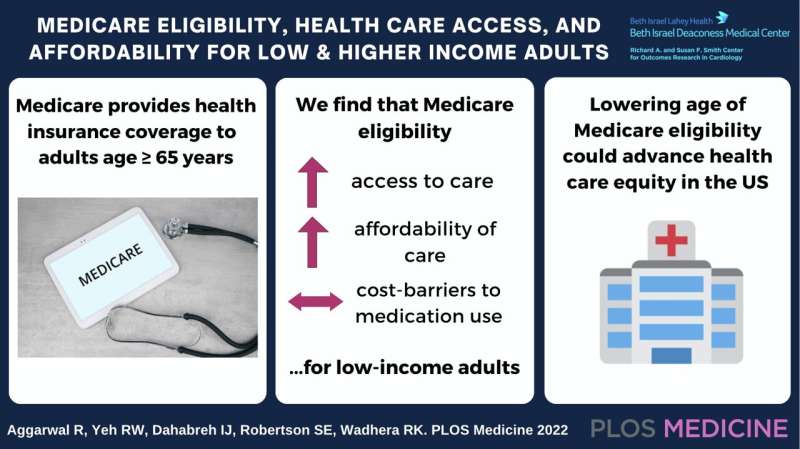
Medicare eligibility and enrollment are associated with decreases in the percentage of low-income adults who delay or avoid medical care due to costs, as well as in the percentage who worry about or have problems paying medical bills, according to a new study publishing on October 4 in the open access journal PLOS Medicine by Rishi Wadhera, of Beth Israel Deaconess Medical Center and Harvard Medical School, U.S., and colleagues.
In the United States, low-income adults are more likely to lack health insurance coverage, face barriers accessing health care, and disproportionately experience financial strain due to health care expenditures compared with higher-income adults. The Medicare program provides health insurance coverage to more than 50 million older adults in the United States.
In the new study, researchers used cross-sectional data from the 2019 U.S. National Health Interview Survey on 1.66 million low-income adults aged 64—just below the Medicare eligibility threshold at age 65—and 1.49 million low-income Medicare-eligible adults, aged 66, with similar baseline characteristics other than age and Medicare eligibility. The study also included a higher-income cohort with 2.11 million adults aged 64 and 2.17 million adults aged 66.
For low-income adults, Medicare eligibility at 65 years was associated with improvements in several areas. Among low-income 64-year-olds, 14.7% delayed care and 15.5% avoided care due to costs, while among low-income 66-year-olds, only 6.2% avoided care and 5.9% delayed care due to costs, decreases of 8.5% (95% CI: -14.7% to-2.4%, P=0.007) and 9.6% (-15.9% to -3.2%, P=0.003).
Similarly, there were significant decreases in measures of financial strain; at age 64, 66.5% of low-income adults were worried about medical bills and 33.9% had difficulty paying medical bills. At age 66, 51.1% worried about and 20.6% had difficulty paying medical bills, decreases of 15.4% (-25.4% to -5.4%, P=0.003) and 13.3% (-23.0% to -3.6%, P=0.007). The findings were more modest and less consistent in higher-income adults. Medicare was not associated with changes in the percentage of low-income or higher-income adults who experienced cost-related barriers to medication use.
“As the debate on whether to lower the age of Medicare eligibility continues in the U.S., policymakers should consider the potential implications of doing so on health care access and affordability for low-income adults, and more broadly, health equity,” the authors say.
Wadhera adds, “More than 40% of US adults below the age of 65 years are either uninsured or inadequately insured. The majority of Americans only become eligible for Medicare insurance coverage at age 65 years, and our findings suggest that this transition is associated with significant improvements in health care access, affordability, and reductions in financial strain for low-income adults, and to a lesser extent, among higher-income adults. As policymakers debate whether to expand the Medicare program, our study provides evidence that lowering the age of Medicare eligibility may advance health equity in the U.S.”
Public Library of Science

