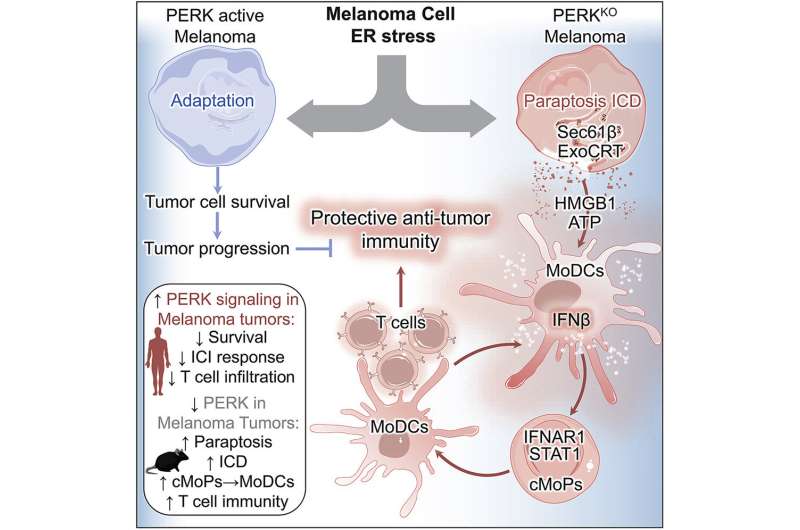
Anti-cancer immune cells are critical to inhibiting the development and progression of tumors, and deregulation of the immune system can limit the ability of immune cells to identify and target cancer cells for destruction. Cancer cells are also subjected to various environmental stresses that impact their survival, such as nutrient deprivation, low oxygen levels and anti-cancer treatments. To continue to survive and overcome these stresses, cancer cells activate survival signaling pathways. PERK is a protein that is activated during stress-induced signaling, but how PERK activation in cancer cells contributes to immune cell evasion is unknown.
Moffitt Cancer Center researchers wanted to determine how PERK activity impacts the clinical outcomes of patients with melanoma. They discovered that patients who had high PERK activity had shorter overall survival than patients who had low PERK activity. Similarly, patients with higher PERK activity had poorer outcomes to immunotherapy and lower levels of anti-tumor immune cells than patients with lower PERK activity.
These observations suggest that PERK may promote survival and impact immune cell activity in patients with melanoma. The authors confirmed this hypothesis in mouse models of melanoma; inhibition of PERK reduced tumor growth in mice, which was dependent on the anti-tumor activity of immune cells. Their results are published in a new article in Cancer Cell.
The researchers performed a series of laboratory experiments to determine the mechanism of how PERK controls immune cells in melanoma. They found that PERK inhibition promotes a type of cell death called paraptosis, which involves swelling of the endoplasmic reticulum and mitochondria and development of fluid-containing vesicles in the cytoplasm of the cell. These cell death-associated immune effects were dependent on the interferon type I proteins. Signaling through interferon type I receptor during PERK inhibition resulted in trafficking of immune cells to tumors and allowed immature immune cells to mature into dendritic cells that triggered anti-tumor T cell immunity.
“Collectively, our results demonstrate the key role of PERK signaling in tumor cells in the evasion of protective immunity. Although these findings predominantly pertain to melanoma, other tumor types may possess a similar susceptibility to PERK-targeted therapy,” explained Paulo Rodriguez, Ph.D., interim chair of Moffitt’s Department of Immunology.
H. Lee Moffitt Cancer Center & Research Institute

