Upon the prick of a finger or scrape of the knee, neutrophils rush to the scene. These white blood cells are the first line of defense against infection in all multicellular organisms. “They are absolutely essential for life,” says Richard Flavell, Ph.D., Sterling Professor of Immunobiology at Yale School of Medicine.
Humanized mouse models, or mice engineered to have a functional human immune system, are a valuable tool for scientists to observe immunobiology in action, but they have limitations. Despite the critical role of neutrophils, no one has been able to study them in a living context. But now, a team of Yale researchers led by Flavell has developed the first humanized mouse model that will allow scientists to study neutrophils in vivo. The team published its findings in PNAS on October 21.
“Neutrophils are involved in almost every immunological disease,” says Esen Sefik, Ph.D., associate research scientist and collaborator on the project. “Our new model will open up many possibilities to a range of scientists studying different diseases.”
To create a humanized mouse model, researchers transfer progenitor cells into the animal that give rise to a human-like immune system that can mimic what would happen in the bodies of human beings when pathogens are present. But in previous mouse models, human neutrophils were unable to grow because they were outcompeted by already-present mouse neutrophils.
Functioning human neutrophils in a living animal
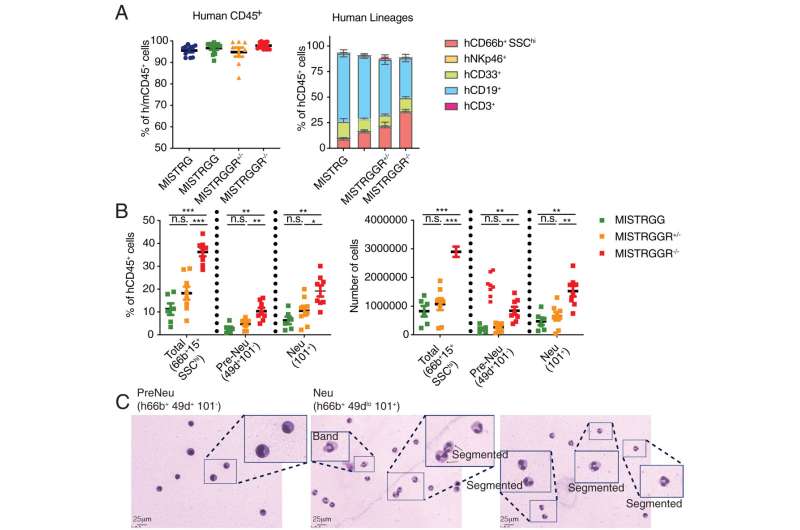
Granulocyte colony-stimulating factor (G-CSF) is a cytokine that promotes the growth and circulation of neutrophils. The binding of G-CSF to its receptor, known as G-CSFR, stimulates this proliferation. In their new mouse model, the team first humanized the cytokine G-CSF. However, they quickly realized that this wasn’t enough—mouse neutrophils continued to dominate. Next, they removed the mouse G-CSF receptors and found that this significantly reduced the numbers of mouse neutrophils in circulation and in the bone marrow.
“We realized that the mouse neutrophils were still detecting and responding to the human cytokine,” says Sefik. “So, we disadvantaged these neutrophils by knocking out the receptor on the mouse cells that responds to G-CSF, thus creating a deficiency in mouse neutrophils and allowing only the human neutrophils to respond to the G-CSF.”
With this discovery, the team wanted to make sure that the human neutrophils were functional in an unperturbed state. They looked at their ability to respond to chemokines and express chemokine receptors, measured the neutrophils’ production of reactive oxygen species, and studied their capacity to create extracellular traps for capturing inflammatory targets. “One by one, we looked at what neutrophils are supposed to do and confirmed they were functioning in a steady state,” says Sefik.
Next, the team tested the ability of the human neutrophils to respond to inflammation. They induced inflammation in the lung using aerosolized lipopolysaccharide (LPS), a component of certain bacteria that can create an acute inflammatory response in tissues, and they found that the neutrophils traveled to the lung in response. They then tested the neutrophils’ response to an active infection by introducing Pseudomonas aeruginosa, a bacterium that predominantly affects immunocompromised individuals and is one of the leading causes of hospital-acquired pneumonia. They found that the neutrophils were able to fight the infection. “We showed that they have the ability to kill bacteria, which is a very important function of neutrophils,” says Sefik.
Finally, the team tested whether neutrophils could mobilize to other parts of the body. They induced inflammation on the skin of the mice and found that the neutrophils mobilized there within minutes. “This shows that our findings were not just a lung phenomenon and that neutrophils can home to any tissue,” says Sefik.
Neutrophils in COVID, cancer, and beyond
The team is not only excited about its scientific achievements, but also its ability to work together through the many obstacles presented by COVID, including time when COVID health protocols kept them out of the lab. “This is not only a nice piece of science, but it’s an example of science done under the very difficult circumstances of the pandemic,” says Flavell. “The victory here is not only the science, but getting the work done under these extremely difficult circumstances. It was an achievement on its own.”
The Flavell lab’s new humanized mice are an unprecedented way to model human neutrophils in a living organism. The investigators hope their work will allow for a greater understanding of these critical white blood cells and their role in a wide variety of diseases. In future studies, the team hopes to study neutrophils in the context of COVID and learn more about how they might contribute to SARS-CoV-2 pathology. They also hope to learn more about the cells’ role in cancer by putting tumors in their humanized mice models and studying the neutrophils’ response.
Isabella Backman, Yale University

