A Rochester Institute of Technology scientist helped develop a new mathematical model that could aid doctors and patients assessing different approaches for treating metastatic cancer. Assistant Professor Nourridine Siewe from RIT’s School of Mathematical Sciences is the lead author on a paper published in the Journal of Theoretical Biology outlining the new method.
In recent years, drugs called immune checkpoint inhibitors have helped advance the treatment of many metastatic cancers, but the treatment only benefits a limited percentage of patients due to immune suppression in the tumor microenvironment. Pairing immune checkpoint inhibitors with other drugs such as anti-PD-1 and anti-CSF-1 could help expand the benefits of the treatment to more patients, but factors such as toxicity levels need to be accounted for as well.
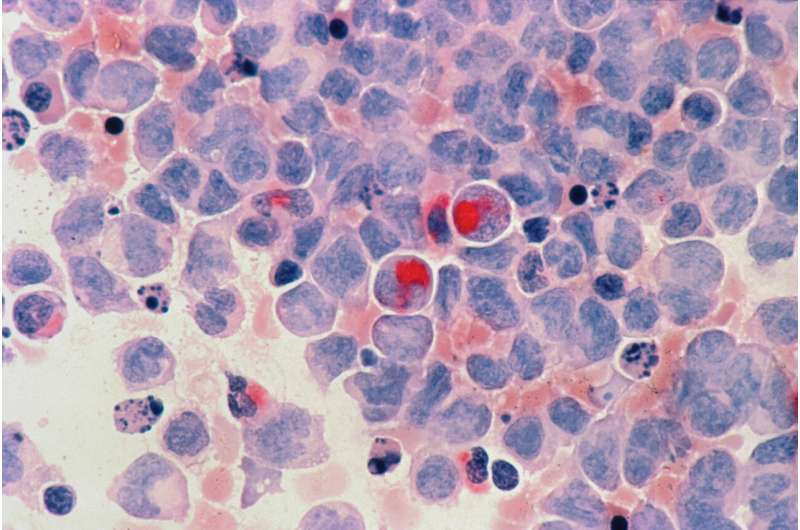
Siewe and his collaborator from The Ohio State University developed a model that shows the interactions among the immune cells and cancer. The model shows how using various drugs at different amounts and points of time impacts the tumor volume and levels of toxicity in the patient. Siewe said he hopes this can be used by the medical field to guide the best opportunities for clinical trials.
“It is very expensive to conduct clinical trials, and this model can help clinicians decide which approaches offer the most favorable conditions,” said Siewe. “Our simulations looked at the tradeoffs between reducing tumor volume and maintaining toxicity at an acceptable level, and we found the best strategy is to give anti-CSF-1 at larger amounts as early as possible.”
Siewe said he hopes to collaborate more with researchers in the medical field in the future to develop similar models for assessing other types of treatments. He also envisions the math model being presented in an app form that allows patients and practitioners to visualize how changing treatment methods can influence tumor volume and toxicity levels.
Luke Auburn, Rochester Institute of Technology

