Cases of scarlet fever in Scotland are “unseasonably high”, according to NHS Borders Health Protection team.
Parents are being asked to be vigilant for symptoms and to seek treatment if they suspect their child has the disease. Because of the highly infectious nature of scarlet fever, those affected are being advised to stay at home for at least 24 hours after beginning antibiotics.
Scarlet fever is a seasonal illness, with cases typically appearing in spring. However, during the first two years of the COVID pandemic, cases dropped significantly, probably due to social distancing, isolation and increased handwashing.
But since the UK dropped these COVID measures, there has been an increase in scarlet fever cases (and other infectious diseases) outside of the usual seasonal occurrences. This is something that is happening globally. It is called the “immunity debt”.
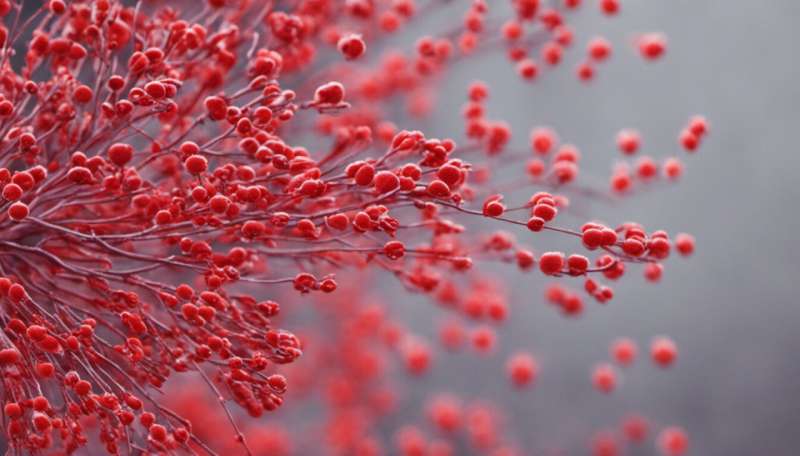
Scarlet fever is caused by streptococcus bacteria. Symptoms typically begin with a sore throat and fever, followed by a telltale red rash on the body and tongue, called “strawberry tongue”.
The bacteria responsible for scarlet fever lives in the nose and throat, and those infected can spread the disease by coughing, talking or sneezing. The bacteria can also spread from touch contact with streptococcal skin infections, such as impetigo.
The disease is most common in children aged between the ages of two and eight years old, with schools and daycare centers being typical sources of exposure. A child with scarlet fever may be uncomfortable for a short time, but with antibiotics, paracetamol and rest they should recover within five days. But this wasn’t always the case.
The path to a cure
Historically, scarlet fever was not a short-term inconvenience to parents and children, but a far more fearful and deadly disease. Between 1900 and 1910 36,000 died of scarlet fever in England and Wales alone. Famously, Charles Darwin’s infant son succumbed to scarlet fever. Of all those who died of scarlet fever, 95% were under ten years of age.
In the 1800s, treatments relied on managing the fever and ensuring the child rested. A research paper from 1835 describes doctors using bloodletting to treat scarlet fever. This involved the withdrawal of blood to “cure” infection.

As of the early 1900s, houses infected with scarlet fever would typically have a brightly colored quarantine sign placed outside to isolate infected people and prevent the further spread of this disease.
It wasn’t until 1924 that husband and wife bacteriologist team, George and Gladys Dick, first identified that the bacteria responsible for “strep throat” released a toxin in the body causing scarlet fever.
Scarlet fever remained an important infectious disease until the introduction of antibiotics in the 1940s. Following Alexander Fleming’s identification of penicillin in 1928, researchers at Oxford University worked to create a pharmaceutical version of penicillin, and in 1941, penicillin was used to treat a streptococcal infection.
Today, penicillin is easily available with a written prescription from a GP in the UK, and a short course of penicillin is effective for treating any new cases of scarlet fever.
Outbreaks still occur
There have been many outbreaks of the disease in the UK in recent decades. Outbreaks were particularly high in 2014 in Yorkshire and the East Midlands, but with penicillin and isolation, they were soon brought under control.
Although we can easily treat scarlet fever, we must still ensure we react to outbreaks with a degree of seriousness. The misuse of antibiotics over previous decades has led to several strains of bacteria becoming resistant to the antibiotics. Previously treatable diseases, such as tuberculosis, are now becoming extremely difficult to treat.
If your child, following a sore throat, develops a red rash with a similar texture to sandpaper, contact your GP. If your child receives a diagnosis of scarlet fever, isolate at home with your child for at least 24 hours after starting antibiotics. And notify your child’s school or daycare center of the diagnosis.
During periods of outbreaks, ensure children are washing their hands often, don’t allow them to share cups with other children, and dispose of used tissues in a bin.
With responsible action, we can control outbreaks and reduce the likelihood of us one day experiencing a penicillin-resistant strain of the scarlet fever bacteria.
Emily Johnston, The Conversation

