Researchers have identified a protein that, when present in high amounts in breast cancer tumors, is an indicator of whether DNA-damaging therapies will work or not.
Lead author of the study, HMRI and University of Newcastle Ph.D. researcher Luiza Steffens-Reinhardt, said this work could lead to more effective chemotherapy for people with breast cancer.
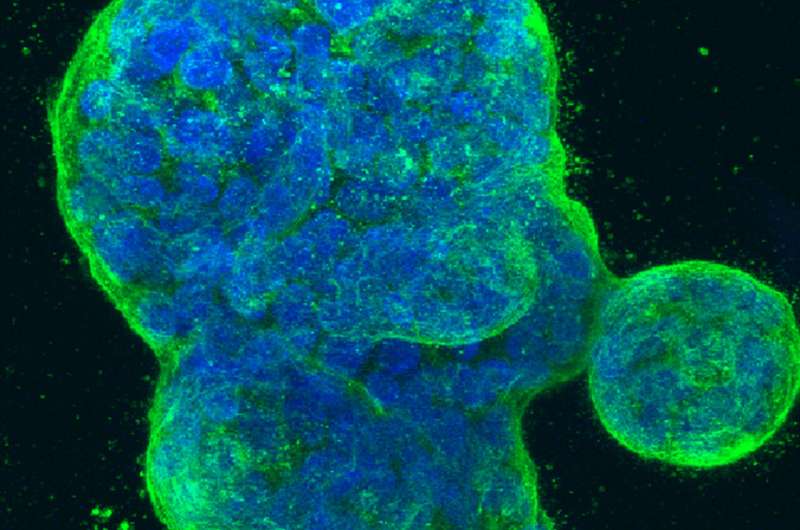
“We looked at this particular variant of a protein called p53 because our previous studies have shown that it is present at high levels in breast cancer and is associated with cancer recurrence,” she said.
“We were surprised to see that by increasing the levels of this variant of p53, the breast cancer cells became unresponsive to existing therapies. Thus, inhibiting this variant could enhance people’s responses to currently used cancer treatments. We recently confirmed these findings in living subjects.”
Breast cancer affects more than 19,000 women every year in Australia and around one-quarter of these people develop treatment resistance.
“The primary reason women die from breast cancer is treatment resistance,” said Ms Steffens-Reinhardt.
“A breast cancer that is resistant to treatment is impossible to cure. Therefore, there is an urgent need to improve therapies that target the cells responsible for resisting these therapies.”
Associate Professor Kelly Avery-Kiejda, who supervises Steffens-Reinhardt on her research, says, this research could be a first step in better targeting breast cancer treatment.
“One in eight women in Australia develop breast cancer and while there is a 92 percent survival rate, this doesn’t take into account secondary cancers or metastasis, which are essentially incurable,” said Associate Professor Avery-Kiejda.
“If we can identify biomarkers that predict how well a patient will respond to certain therapies, we can then target the available therapies more effectively.”
The findings were published in a paper titled ‘Alterations in the p53 isoform ratio govern breast cancer cell fate in response to DNA damage’ in the Cell Death & Disease journal.
This paper is the culmination of investigative work that Associate Professor Avery-Kiejda started in 2009.
This research builds on foundation research that was conducted with the generous support of the Cancer Institute NSW and the Estate of the late Joy Heather Granger.
Hunter Medical Research Institute

