The most comprehensive study of kidney cancer at single-cell level has discovered a potential drug target to treat renal cell carcinoma, a cancer with a high mortality rate that is hard to detect. Researchers from the Wellcome Sanger Institute, the University of Cambridge and Cambridge University Hospitals identified immune cells known as macrophages that express the gene IL1B as crucial to tumor development.
The study, published today in Cancer Cell, recommends IL1B macrophages as a promising therapeutic target to treat renal cell carcinoma given that this cell type has already been targeted using existing drugs that prevent lung cancer. The next step, which is already being explored, will be clinical trials to prove that targeting IL1B can be used to effectively prevent renal cell carcinoma from forming or progressing.
Renal cell carcinoma (RCC) is the seventh most common cancer in the UK, with three quarters of cases and the majority of deaths caused by clear cell renal cell carcinoma (ccRCC). The disease has a 50% mortality rate, partially because three in five patients show no symptoms until the cancer is at a late stage.
Many RCC tumors form when both copies of the VHL gene are switched off. A subset of patients have inherited kidney cancer, including Von Hippel-Lindau (VHL) disease, which is a genetic condition where one copy of the VHL gene is switched off from birth. The second copy of VHL is usually switched off as a result of a common genetic event that often occurs in early life, leading to the formation of innumerable tumors.
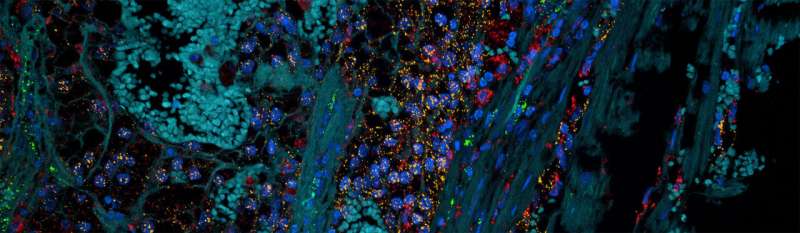
In this new study, researchers at the Wellcome Sanger Institute and University of Cambridge studied over 270,000 single cells and 100 micro-dissections from 12 patients with kidney tumors. Samples were taken from different parts of the tumor as well as normal kidney tissue. These samples were analyzed using single-cell RNA sequencing and spatial transcriptomics to map the exact location of specific cells within tissues.
This analysis highlighted a particular type of immune cell, a macrophage expressing the gene IL1B, as abundant at the fringes of tumors.
“Using both single-cell sequencing and spatial transcriptomics allowed us to discover not only what cell types were present in these renal cell carcinoma tumors, but how the cell types were organized in space. This approach meant we could pinpoint macrophages expressing the IL1B gene at the leading edges of tumors, acting almost like a vanguard for tumor growth,” says Dr. Ruoyan Li of the Wellcome Sanger Institute.
The findings will be of particular interest to those with VHL disease, who are highly likely to suffer numerous and persistent tumors. While kidney tumors can be monitored and surgically removed before the cancer can spread to other parts of the body, new ones will form and there is a limit to how many times patients can have surgery before losing kidney function.
“As a result of research, the outlook for those living with VHL disease has improved greatly in recent years. Even before the VHL gene was identified, the standard of care has always been a lifetime of surveillance with frequent, painful, and expensive surgeries to remove tumors interspersed within the body,” says Joshua Mann, MPH, director of health, VHL Alliance.
“We are approaching a new era of managing VHL disease, with a major paradigm shift that could eventually even do away with these surgeries. A way to treat VHL-related tumors without surgical intervention would be a huge boost for those with the condition. The VHL Alliance is actively exploring opportunities to bolster and support these important research efforts.”
The researchers are already planning clinical trials to test whether targeting IL1B macrophages is an effective treatment for RCC. The fact that existing drugs targeting this pathway are proven to be effective in preventing some lung cancers offers hope that these trials may deliver promising results.
“I’m optimistic that targeting IL1B macrophages may provide us with a way to treat renal cell carcinomas without resorting to surgery. This will be particularly important for patients with VHL disease because we should be able to prevent tumors forming in the first place by focusing on their genetic roots, rather than waiting for them to grow and removing them. As is the case for all cancers, the earlier we can intervene the better,” says Dr. Thomas Mitchell, Wellcome Sanger Institute and University of Cambridge.
Wellcome Trust Sanger Institute

