Using machine learning and clinical data from electronic health records, researchers at the Icahn School of Medicine at Mount Sinai in New York constructed an in silico, or computer-derived, marker for coronary artery disease (CAD) to better measure clinically important characterizations of the disease.
The findings, published online on December 20 in The Lancet, may lead to more targeted diagnosis and better disease management of CAD, the most common type of heart disease and a leading cause of death worldwide. The study is the first known research to map characteristics of CAD on a spectrum. Previous studies have focused only on whether or not a patient has CAD.
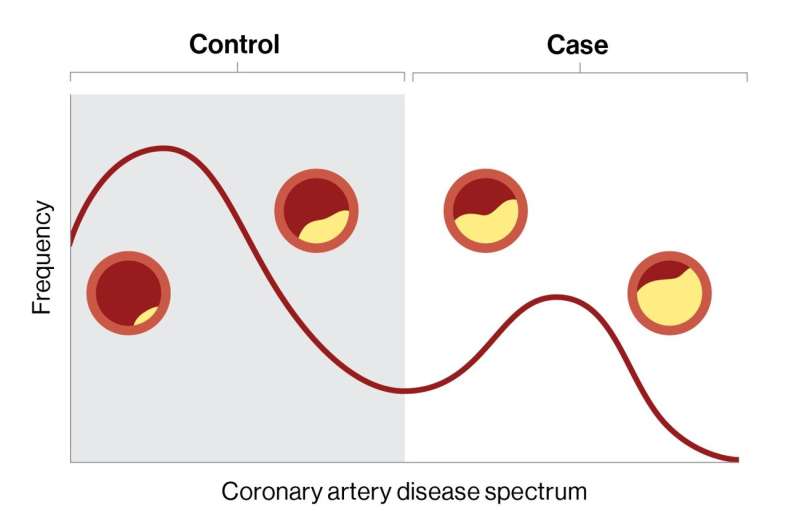
CAD and other common conditions exist on a spectrum of disease; each individual’s mix of risk factors and disease processes determines where they fall on the spectrum. However, most such studies break this disease spectrum into rigid classes of case (patient has disease) or control (patient does not have disease). This may result in missed diagnoses, inappropriate management, and poorer clinical outcomes, say the investigators.
“The information gained from this non-invasive staging of disease could empower clinicians by more accurately assessing patient status and, therefore, inform the development of more targeted treatment plans,” says Ron Do, Ph.D., senior study author and the Charles Bronfman Professor in Personalized Medicine at the Icahn School of Medicine at Mount Sinai.
“Our model delineates coronary artery disease patient populations on a disease spectrum; this could provide more insights into disease progression and how those affected will respond to treatment. Having the ability to reveal distinct gradations of disease risk, atherosclerosis, and survival, for example, which may otherwise be missed with a conventional binary framework, is critical.”
In the retrospective study, the researchers trained the machine learning model, named in silico score for coronary artery disease or ISCAD, to accurately measure CAD on a spectrum using more than 80,000 electronic health records from two large health system-based biobanks, the BioMe Biobank at the Mount Sinai Health System and the UK Biobank.
The model, which the researchers termed a “digital marker,” incorporated hundreds of different clinical features from the electronic health record, including vital signs, laboratory test results, medications, symptoms, and diagnoses, and compared it to both an existing clinical score for CAD, which uses only a small number of predetermined features, and a genetic score for CAD.
The 95,935 participants included participants of African, Hispanic/Latino, Asian, and European ethnicities, as well as a large share of women. Most clinical and machine learning studies on CAD have focused on white European ethnicity.
The investigators found that the probabilities from the model accurately tracked the degree of narrowing of coronary arteries (coronary stenosis), mortality, and complications such as heart attack.
“Machine learning models like this could also benefit the health care industry at large by designing clinical trials based on appropriate patient stratification. It may also lead to more efficient data-driven individualized therapeutic strategies,” says lead author Iain S. Forrest, Ph.D., a postdoctoral fellow in the lab of Dr. Do and an MD/Ph.D. student in the Medical Scientist Training Program at Icahn Mount Sinai.
“Despite this progress, it is important to remember that physician and procedure-based diagnosis and management of coronary artery disease are not replaced by artificial intelligence, but rather potentially supported by ISCAD as another powerful tool in the clinician’s toolbox.”
Next, the investigators envision conducting a prospective large-scale study to further validate the clinical utility and actionability of ISCAD, including in other populations. They also plan to assess a more portable version of the model that can be used universally across health systems.
The Mount Sinai Hospital

