A global study led by the University of Otago has discovered a gene, that when modified, could reduce the risk of breast cancer. The paper is published in the journal Communications Biology.
The discovery, led by Associate Professor Logan Walker, of the Department of Pathology and Biomedical Science, Christchurch, also opens the door to the development of a risk-reducing drug—a project that will also be led by Otago University.
The initial study was the world’s largest of women known to have mutations of the breast cancer genes—BRCA1 and BRCA2. It made two “significant” discoveries.
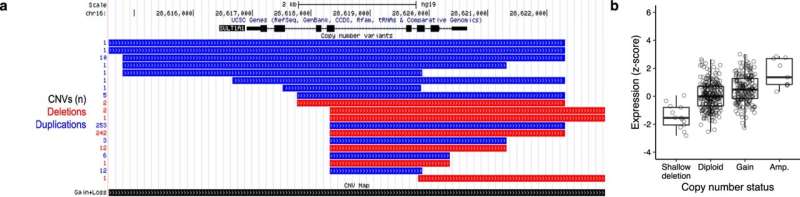
“We have found a gene—the SULT1A1—that may help doctors decrease the chance of women getting breast cancer, especially if they have also inherited a mutation in the BRCA1 gene,” Associate Professor Walker says. “We have also found that women who have inherited a BRCA1 gene with segments missing are, for reasons as yet unknown, at the highest risk of developing breast cancer.”
The study, in collaboration with the international Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA), involved about 26,000 women known to have mutations in the BRCA1 or BRCA2 genes, and 166 researchers from 160 institutes worldwide.
In New Zealand, about one in every 250 individuals inherit a genetic mutation in these two genes, which means they are at high risk of developing breast and ovarian cancer. However, the risk of cancer for these individuals varies significantly due to other unknown genetic changes, creating a significant challenge for counseling and clinical decision making.
Currently, the most effective risk-reducing strategy for these women at high risk of breast cancer is a bilateral mastectomy. Although effective, this approach is irreversible and can cause ongoing psychological and physiological harm to patients, especially for younger women, Associate Professor Walker says.
The study found that reduced levels of the protein produced by the SULT1A1 gene, that plays an important role in the metabolism of cancer-causing agents, lowered the risk of breast cancer.
“When we turned down the activity of the SULT1A1 gene in breast cells, the cells grew more slowly and were more resistant to DNA damage. This anti-cancer-like feature supported epidemiological results from 26,000 women,” he says.
The next step is developing a risk reducing drug—a project to be led by Otago’s Dr. George Wiggins.
“Prophylactic drug treatments are becoming well-established for the prevention of different diseases. For example, aspirin, statins and anti-hypertensive therapies have had a major impact on reducing incidence of cardiovascular disease and extending life expectancy,” he says.
“By comparison, progress in therapeutic intervention to prevent breast cancer has been poor. Providing a non-invasive and easily accessible preventative therapy for women at high risk of developing breast cancer would have numerous benefits for the health system, and for the patients and their whānau [extended family].
“Such a therapy could give genetically predisposed young women the opportunity to bear and breastfeed their children by delaying or supplanting the need for risk-reducing surgery,” Wiggins continues.
In New Zealand, breast cancer is the most commonly diagnosed cancer in Māori and non-Māori women, with more than 3,300 individuals diagnosed and more than 600 deaths per year.
“Uptake of risk reducing surgery can also be a barrier to breast cancer prevention for many individuals, contributing to inequity in health outcomes,” Associate Professor Walker says. “Effective prevention strategies for women at increased risk of breast cancer are vital for controlling and reducing the social and economic impact of this disease.”
University of Otago

