Northwestern Medicine investigators have revealed new insights into how cancer cells can change their form by undergoing phenotypic “switches” to facilitate tumor growth and treatment resistance in small cell lung cancer, according to findings published in Science Advances.
“This cancer can substantially shape shift or morph, utilizing at least three distinct cell types or developmental programs. The current standard of care therapies for this tumor mainly targets the neuroendocrine subtype of cells, leaving the others to linger and rapidly repopulate the tumor when therapy is ultimately stopped,” said Mohamed Abazeed, MD, Ph.D., associate professor of Radiation Oncology and senior author of the study.
An estimated 15% of all lung cancer cases diagnosed worldwide are small cell lung carcinomas. The cancer typically develops in patients with a significant history of tobacco consumption and has a 5-year survival rate of just 6%, with most patients dying from the disease within a year of diagnosis.
While most patients respond to first-line therapy, which often includes a combination approach of chemotherapy and radiation therapy, many will also relapse. The need for more effective targeted therapies is urgent, according to Abazeed, but progress has remained slow.
“The disease is aggressive with very little progress in the last four decades. It’s also not amenable to surgical resection, so that makes collecting research samples for investigational studies quite difficult,” said Abazeed, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
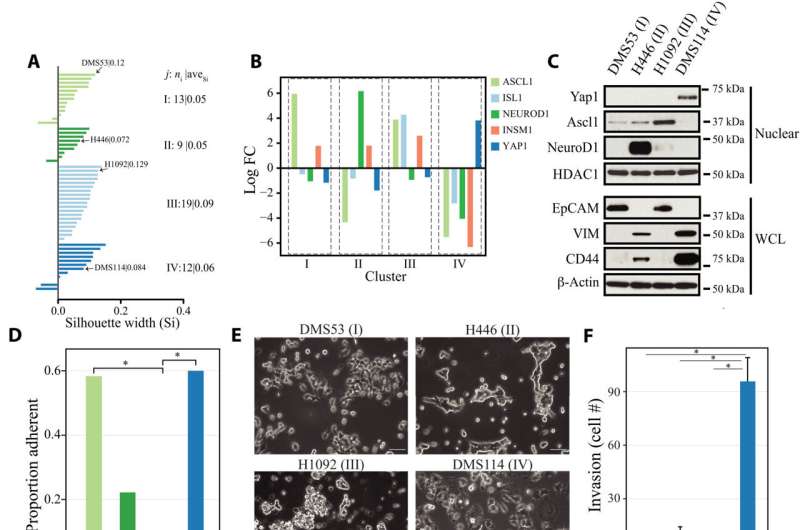
More recently, investigators have begun to successfully develop patient-derived xenograft models of small cell lung carcinoma, which allow for further investigation. In the current study, Abazeed’s team studied the profiles of more than 60 of these models using multiple omics platforms.
In these samples, the investigators found that the cancer cells were substantially more heterogeneous than previously appreciated, suggesting that some of the more commonly used cancer cell lines may have evolved into more discrete cell types.
“That suggested we were missing a substantial extent of the intratumoral heterogeneity in individual samples due to these less-than-optimal cellular systems,” Abazeed said.
The investigators also used high-resolution microscopy to observe when the cancer cells converted into different cell types. Furthermore, they found the cells contained a high level of plasticity, allowing the cells to convert into different cell types to achieve “cell state equilibrium” and promote tumor growth and treatment resistance.
“All the cancer has to do is maintain a proportion of the cell types that are resistant to chemotherapy, and once the chemotherapy is no longer present, then it can convert back and repopulate very quickly,” Abazeed said.
Using epigenetic targeting drugs, the investigators also identified previously unknown mechanisms that help the cancer cells switch their epigenetic programming. Furthermore, modulating these switches with epigenetic drugs could slow tumor growth or stall cancer recurrence, according to Abazeed.
“There’s this a coordinated set of events that are happening during these cell type switches, and I think understanding the zeitgeber or time cue and the molecular cascade that leads to these transitions will reveal some fundamental insights into cell type switches in cancer and beyond,” Abazeed said.
Melissa Rohman, Northwestern University

