For up to 40 years, nearly 800,000 people from Sweden, Norway and Austria have been tracked based on how their BMI and metabolic health—that is, their blood pressure, blood glucose levels and blood fats—affect the risk of suffering from obesity-related cancers. The study shows that those who are metabolically unhealthy are at a higher risk of certain forms of cancer, regardless of their body weight.
It is already known that obesity is linked to more than ten different cancers. Now researchers in a European collaboration run by Lund University have studied how metabolic health interacts with body weight in relation to the risk of obesity-related cancer.
In a study now published in the Journal of the National Cancer Institute, the researchers included data from health surveys and national registries from nearly 800,000 individuals through the years 1972-2014.
By weighing together data on blood pressure, blood glucose and blood fats in the form of triglycerides, they produced a metabolic score that determined whether the people were considered metabolically healthy or unhealthy. Based on BMI (Body Mass Index), the participants were also divided into the categories of normal weight, overweight or obese.
“Being metabolically unhealthy is often linked to obesity, but you also don’t have to be overweight to have a metabolically unhealthy status. Therefore, it is relevant to study how this status plays a role in the relationship between BMI and obesity-related cancer,” says Tanja Stocks, epidemiology researcher who led the study.
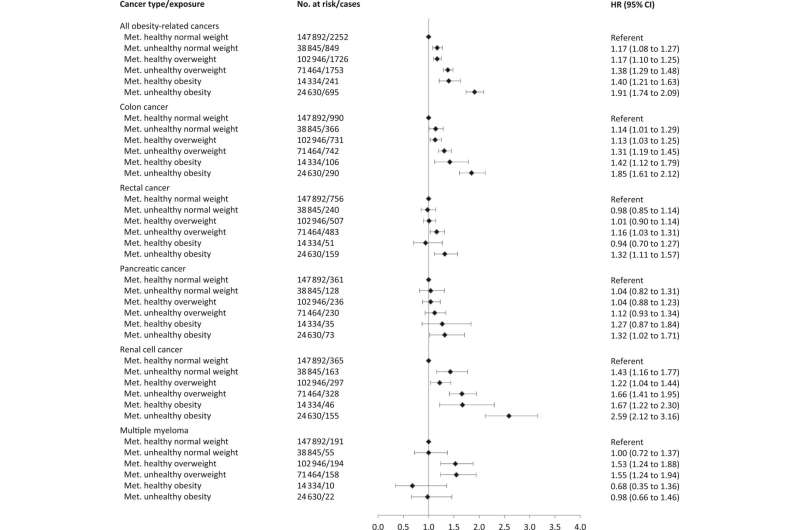
During the follow-up period of up to 40 years, 23,630 individuals were diagnosed with an obesity-related cancer. It was no surprise to the researchers that a higher BMI increased the risk of cancer, but being metabolically unhealthy was also associated with an increased risk.
The highest risk was found among individuals with metabolically unhealthy obesity, which was associated with the highest risk for cancer of the liver, kidney, and among women also for endometrial cancer. Another important finding was that metabolic unhealth in itself represented an increased risk of obesity-related cancer—regardless of whether one was of normal weight, overweight or obese.
The study cannot prove causation, but the researchers did see that obesity and metabolic disease interacted in a way that increased the risk of certain cancers more than expected when the two factors were combined.
“The study shows the importance of assessing different metabolic risk profiles in addition to obesity, in order to be able to identify the groups that can benefit most from interventions to reduce their risk of suffering from obesity-related cancers,” concludes Ming Sun, Ph.D. student and first author of the study.
Lund University

