Isolated REM-sleep behavior disorder is a condition that can provide an indication of Parkinson’s disease well in advance. A research team headed by Professor Dr. Erdem Gültekin Tamgüney from Heinrich Heine University Düsseldorf (HHU) has shown that a greater concentration of α-synuclein aggregates can be detected in the stool samples of sufferers.
In the journal npj Parkinson’s Disease, they now present a method for detecting these aggregates, which they have developed in collaboration with the University Hospital Cologne, Jülich Research Center (FZJ) and the company attyloid GmbH.
There are two forms of Parkinson’s disease (for short: PD). In 70% of cases, it originates in the central nervous system. However, in around 30% of cases it originates in the nervous system of the intestine (“enteric nervous system”). The latter form is referred to as “body-first Parkinson’s disease” (for short: body-first PD) and the characteristic deposits of aggregates of the body’s own α-synuclein protein are formed in the neurons in the intestine.
A preliminary form of body-first PD is isolated REM-sleep behavior disorder (for short: iBRD). It causes in part complex movements during a specific phase of sleep—REM-sleep—insofar as the patient experiences vivid and disturbing dreams. These movements can endanger the sufferer themselves or others.
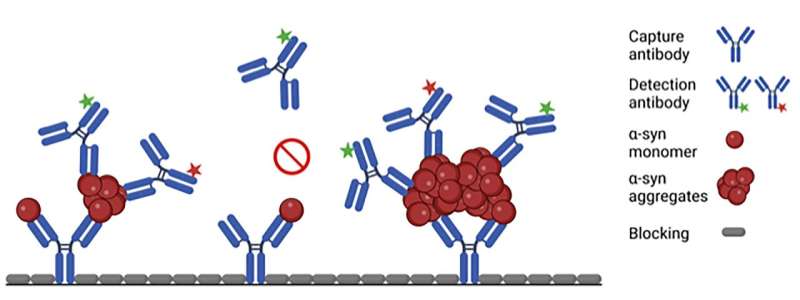
A research team headed by Professor Erdem Gültekin Tamgüney from the Institute of Physical Biology at HHU now reports that it is possible to detect an elevated level of α-synuclein aggregates in the stool samples of patients. To achieve this, the team used a new surface-based fluorescence intensity distribution analysis (sFIDA) to detect and quantify individual particles of α-synuclein aggregates.
Professor Tamgüney says, “We are the first to prove the presence of α-synuclein aggregates in stool samples. Our results show a significantly higher level of α-synuclein aggregates in iRBD patients compared with healthy individuals or patients with Parkinson’s. These findings could lead to a non-invasive diagnostic tool for prodromal synucleinopathies—including Parkinson’s—which could in turn enable therapies to be initiated at an early stage before symptoms occur.”
However, more research is required before the process can find its way into clinical practice, for example investigation into why the level is lower in Parkinson’s patients.
The study was conducted in collaboration with the Institute of Biological Information Processing—Structural Biochemistry (IBI-7) at Jülich Research Center (FZJ), the Department of Neurology at the University Hospital Cologne and the HHU/FZJ spin-off attyloid GmbH. HHU worked with the University Hospital Cologne to establish a biobank with stool samples from patients and control subjects, and with FZJ to develop the test procedure and conduct the tests on the samples. attyloid GmbH is a cooperation partner and is working towards the commercial exploitation of the results. It is necessary to verify that the test procedure is safe and can be used in normal operations in order to gain a license.
In body-first PD, the deposits of fibrils of the body’s own α-synuclein protein, which are characteristic of Parkinson’s, are first formed in the neurons of the enteric nervous system, which serves the gastrointestinal tract. The aggregates then spread to the central nervous system in a way similar to prions, i.e. an existing aggregate combines individual α-synuclein proteins in its vicinity into further aggregates in a nucleation process; these aggregates then spread further through the body.
The influence of what happens in the gastrointestinal tract on the brain is referred to as the “gut-brain axis.” The gastrointestinal tract is exposed to the environment and it is possible that harmful substances such as chemicals, bacteria or viruses ingested directly with food or via interaction with the microbiome of the gastrointestinal tract may trigger the pathological formation of α-synuclein aggregates.
Heinrich-Heine University Duesseldorf

