The bones of the face and skull can be affected due to a wide range of conditions, including cleft palate defects, traumatic injuries, cancer, and bone loss from dentures. Although bone replacements are routinely used to regenerate the missing tissue, they are vulnerable to bacterial infection. In a new study, researchers investigated whether manuka honey, made from tea trees, can be used to resist bacterial infection and promote bone growth.
Bone implants account for 45% of all hospital-contracted infections, impeding healing. Typically, these implants are made from biomaterials that contain extracellular matrix components—molecules that provide structural support to cells. However, researchers commonly use metal implants or synthetic polymers to study bone defects and infections. Therefore, there is a gap in the understanding of how biomaterials behave in response to infection.
“Imagine a metal versus something soft and porous that is made up of extracellular matrix components. They have very different characteristics,” said Marley Dewey, a former graduate student in the Harley lab and the first author of the paper. “Using our scaffolds, this is the first paper to look at how these materials become infected.”
The researchers used collagen scaffolds to study whether manuka honey can be incorporated to inhibit the growth of Pseudomonas aeruginosa and Staphylococcus aureus, two bacteria that commonly infect bone wounds.
“At various conferences I saw researchers talk about how nature-derived materials can be used instead of antibiotics, circumventing the problem of antibiotic resistance. Additionally, when I looked at the literature, I found research that claimed manuka honey can be useful,” Dewey said.
In the study, the researchers added the manuka honey into the scaffolds in two different ways: incorporation and soaking. In the first method, they added the honey to a collagen suspension and blended them together. The suspension was then used to create scaffolds that had honey embedded in their structure. In the second process, the prepared collagen scaffolds were soaked in manuka honey for 40 hours. In both cases they tested whether the addition of manuka honey had an effect on bone growth and bacterial infection.
“We focused on characterizing the mesenchymal stem cell response, which is important for bone repair since these cells differentiate to create bone,” Dewey said. “We first tested different concentrations of honey to find the ideal concentration we need to use.”
They found that when the scaffolds were soaked in 5% honey, there was higher mineral formation and osteoprotegerin production, all pointing to increased bone production. Higher concentrations of honey, however, led to a decrease in bone health. Furthermore, the soaked scaffolds worked better than the incorporated ones, although the reason is unclear.
Next the researchers tested whether the growth of P. aeruginosa and S. aureus is inhibited by manuka honey. To do so, they soaked paper discs in different concentrations of honey and added them to bacterial lawns. To their surprise, none of the concentrations were able to prevent bacterial growth. Similarly, the honey-soaked scaffolds were unable to prevent bacterial growth, even though the bacteria were not able to attach to these surfaces.
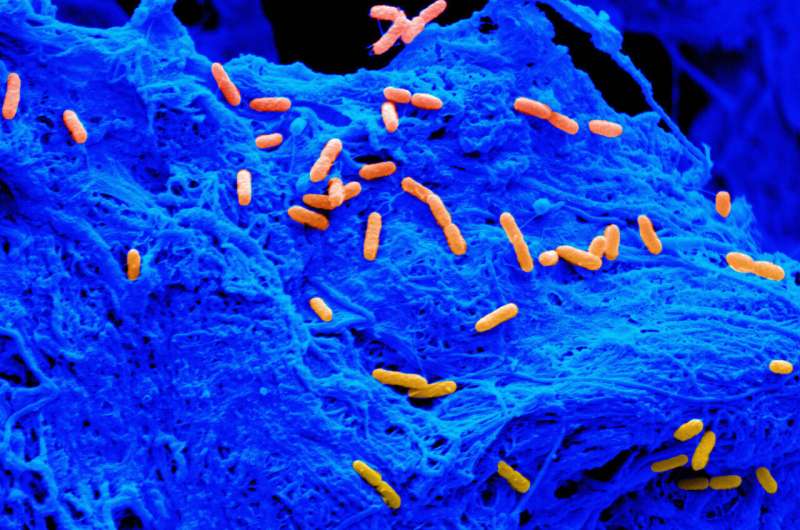
“We measured bacterial growth with scanning electron microscopes; by using representative images, we were able to count the number of bacteria,” Dewey said.
Due to claims in the literature, the researchers had initially hoped that adding antibiotics would help inhibit bacterial growth. However, once again, they were surprised. “It was striking that we needed ten times the amount of antibiotics to kill the bacteria and some still survived,” Dewey said. “It’s possible that it is easy to kill the bacteria when metal implants are used. However, our collagen scaffolds seem to offer a protective environment for bacteria, creating a big problem.”
Dewey hopes to establish her own lab soon where she will continue working on how biomaterials can be used to prevent infection. “I want to create models that other people can use for implant infection. I’m also interested in understanding how bacteria interact with cells in the scaffolds and why they are so resistant to antibiotics in a scaffold structure,” Dewey said.
“This work was made possible with the help of the IGB themes,” said Brendan Harley (RBTE leader/EIRH), Robert W. Schaefer Professor of Chemical and Biomolecular Engineering. “Bringing in Alan Collins, a member of IGOH, was essential in the bacterial culture work. He helped us gain the expertise we needed to complete this study.”
The study “Evaluation of bacterial attachment on mineralized collagen scaffolds and addition of manuka honey to increase mesenchymal stem cell osteogenesis” was published in Biomaterials.
University of Illinois at Urbana-Champaign

