A new study in The EMBO Journal has revealed how fat tissues might provide a protective role in intestinal inflammation opening new lines of research into the treatment of inflammatory bowel diseases.
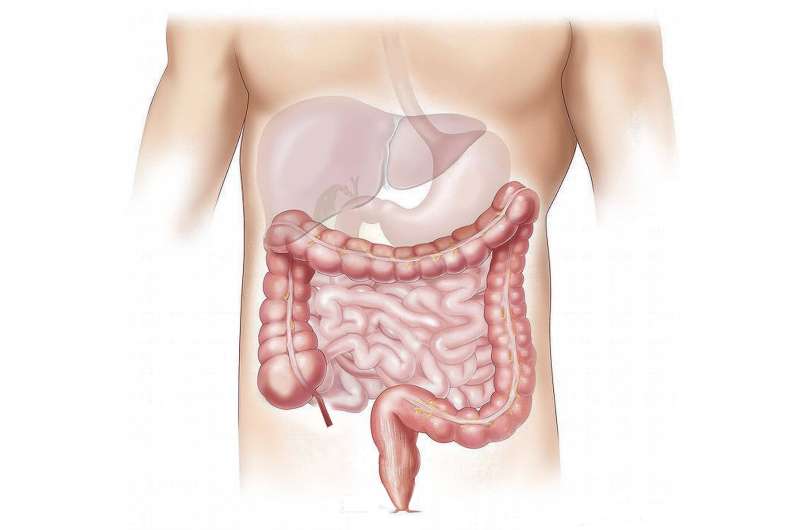
A fraction of inflammatory bowel disease (IBD) patients, predominantly those with Crohn’s disease, develop a phenomenon known as creeping fat tissue over the course of their condition. This describes the wrapping of fat around the inflamed part of the intestine. Its biological function, whether beneficial or maladaptive however, remains unclear.
The results have revealed a novel crosstalk between fat tissues and the intestine suggesting that fat tissues, at least initially, may have a protective and beneficial effect by preventing excessive intestinal inflammation.
Lead author Felix Richter said, “We were interested to study the crosstalk between fat tissues and the intestine during intestinal inflammation. We focused our efforts on the role of autophagy, a recycling pathway for cell components, in fat cells and how this would influence the inflammatory processes during colitis. Mutations or disruption of genes in the autophagy pathway have been previously associated with higher susceptibility to IBD, and Crohn’s.”
The study showed that intestinal inflammation induces autophagic flux in adipose tissues of mice and creeping fat of Crohn’s disease patients. It identified that fat tissues increase the secretion of the anti-inflammatory cytokine IL-10 during intestinal inflammation. However, a genetic deletion of the autophagy pathway prevented this additional adipose tissue-derived IL-10 secretion, and led to more severe intestinal inflammation.
“We found that autophagy seems to be an important modulator of adipose tissue homeostasis by controlling the production of important signaling lipids which regulate the production of IL-10 from adipose tissue macrophages during intestinal inflammation,” said Katja Simon, Professor of Immunology at the Kennedy Institute and MDC Berlin “The role of these signaling lipids is being investigated as possible therapeutics for IBD patients and our study adds to their possible beneficial effects.”
University of Oxford

