Lung cancer patients can have their risk of dying accurately predicted within the last four weeks of life, a study involving University of Liverpool researchers has shown.
By analyzing the urine of patients, it is possible to accurately determine their likelihood of death, allowing them and their families to better prepare for their end of life and giving clinicians more information to inform their care and medication plans. This method can also allow for timely stoppage of potentially invasive tests and treatments, and a move to peaceful palliative care.
In a paper published in the International Journal of Molecular Sciences, the researchers show how metabolic changes taking place during the 30 days ahead of a patient dying can be measured to predict date of death, with accuracy increasing as the time of death nears.
Co-author Professor Chris Probert, a consultant gastroenterologist at the Royal Liverpool University Hospital and Professor of Gastroenterology at the University of Liverpool, said, “Nearly 10 million people worldwide died from cancer in 2020 and lung cancer, with the highest mortality, was responsible for 1.8 million deaths.
“Predicting when patients with advanced cancer are likely to die is challenging and no accurate test is available to determine this. However, early recognition that a person may be dying is central to all the priorities for improving people’s experience of care in the last days and hours of life.
“This is the first study to use a metabolomics approach to investigate the dying process in the last weeks of life. The findings provide evidence to support the hypothesis that there are specific metabolic changes associated with the dying process in cancer.”
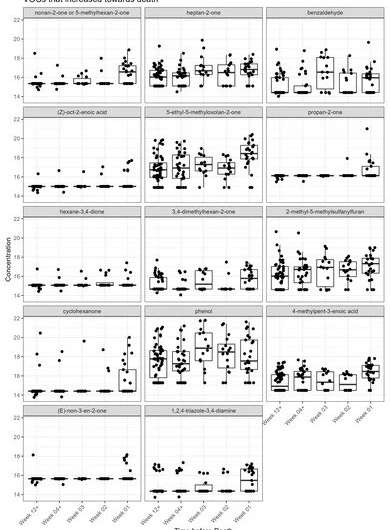
There are common biomarkers that have been identified in patients dying from cancers, and the researchers have specifically identified changes in volatile organic compounds. They analyzed urine from 144 patients with lung cancer in the last few weeks of life using gas chromatography mass spectrometry and identified clear metabolic changes associated with end of life.
Thirty-seven volatile organic compounds were shown to change to such an extent that significant predictions of death could be made, stratifying patients into having a low, medium and high risk of dying. The results within 30 days were shown to have “excellent” probability values.
Co-author Dr. Seamus Coyle, consultant in palliative medicine at The Clatterbridge Cancer Center, an Honorary Senior Clinical Lecturer at the University of Liverpool and Cancer Sub-Speciality Lead for Palliative Care Research at the NIHR Clinical Research Network: North West Coast, said, “By studying volatile organic compounds in urine we have created a model to predict with high probability when these patients will die.
“Knowing when a patient is likely to die is the start of good end of life care and allows for families and patients to plan more accurately and to support their loved one through the dying process. It also better informs clinicians so they can make more appropriate decisions about the patient.”
The researchers propose that this can be used as a tool to inform clinicians as they make end-of-life predictions for a patient suffering from terminal lung cancer.
The Clinical Research Network: North West Coast provided staff and resource to deliver this study. The Network’s Clinical Director, Professor Enitan Carrol said, “The passing of a loved one is such a difficult time for families and carers. This study is of fundamental importance in helping clinicians to support people and their families in their last few days of life.
“We are grateful to all the researchers, patients and family members who took part to make this possible. We are very proud to see palliative care research from our region making a global impact.”
The metabolic changes the team have identified are specific to terminal lung cancer, and the team hope that future research into other terminal cancers, or even patients in critical care settings, will identify the biomarker changes and help to inform predictions. The team already have further studies underway to verify their model.
University of Liverpool

