Treatment is scarce for functional neurological disorder (FND), which requires a multidisciplinary approach. A special report published in the March/April issue of Harvard Review of Psychiatry (HRP) aims to show clinicians and institutions around the world what is needed to establish effective community treatment programs for FND, as well as hospital inpatient and outpatient interventions, in their own health care settings.
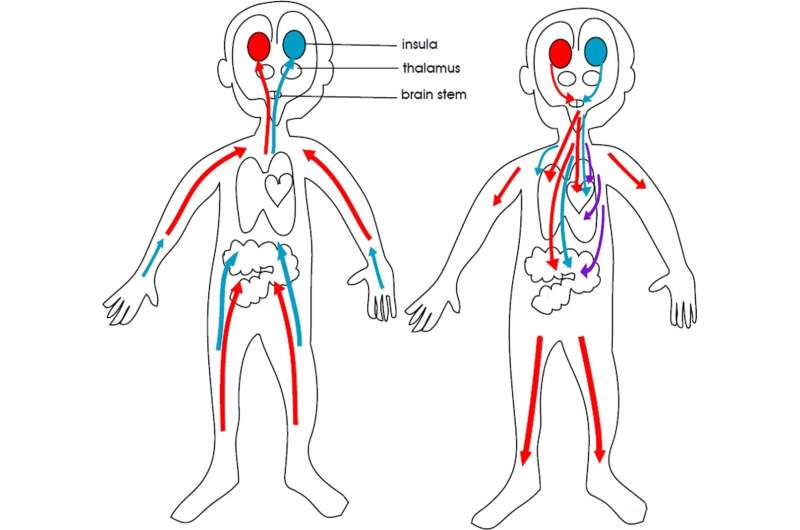
Functional neurological disorder, formerly called conversion disorder, involves the biological embedding of lived experience in the body and brain. This is the process whereby stress, the social environment, or early experience affects the body’s biological systems. The embedding culminates in stress-system activation or dysregulation and aberrant changes in neural network function.
Patients with FND have neurologic symptoms such as limb weakness, tremors, gait difficulties, seizures, or cognitive problems that are not explained by traditional neurological disorders.
As many as a fifth of children and adolescents seen in pediatric neurology clinics are found to have FND. An estimated 63% to 95% of these patients can fully recover if they receive prompt diagnosis and proper treatment.
A treatment gap exists worldwide for pediatric patients with FND
Unfortunately, many children with FND do not receive the care they need. Kasia Kozlowska, MD, Ph.D., a child and adolescent psychiatrist at The Children’s Hospital at Westmead in Sydney, Australia, and colleagues explain the scarcity of treatment is global, in part “the result of long-standing stigma and ingrained belief that patients with FND do not suffer from a real (‘organic’) disorder and that they therefore do not require, or even deserve, treatment.”
In a Perspectives article in HRP, Dr. Kozlowska and her colleagues describe the elements of a biopsychosocial mind–body program intervention they designed that has been successful for managing FND in children and adolescents.
A seven-component treatment program
Over almost 30 years, the Mind–Body Program for children with FND at The Children’s Hospital at Westmead has delivered inpatient care to hundreds of patients with FND. In collaboration with community-based clinicians, the program’s staff has also designed individualized treatment for hundreds of outpatients.
The authors say that although care is personalized, their interventions for FND always have seven elements: prompt medical/neurological assessment and diagnosis by a physician; triaging the referral for a holistic (biopsychosocial) assessment; a holistic, biopsychosocial assessment of the child and family; co-constructing a formulation with the child and family to identify factors that contribute to and maintain the child’s symptoms; assembling a personalized treatment plan; implementing the plan; and building resilience and preventing relapse.
The article describes each of these elements in detail.
Most health care professionals working in pediatrics can easily add an FND-informed skill set to their current clinical practice, Dr. Kozlowska’s group notes:
- Pediatricians and pediatric neurologists already have the skills necessary to diagnose FND: they simply need to learn to recognize the rule-in signs for FND and to practice communicating an FND diagnosis.
- Physical therapists can shift their approach from a “musculoskeletal framework that focuses attention on the problem area” to a framework in which the patient’s attention is drawn away from the symptoms, with particular focus on building a therapeutic relationship, using play, and applying interventions in ways that address the problem indirectly.
- Mental health clinicians already know how to conduct a biopsychosocial assessment and provide individual and family interventions; they just need to understand “the somatic narrative,” the bottom-up approach to emotion regulation, and strategies for managing focus of attention.
Dr. Kozlowska and colleagues emphasize that FND is a positive diagnosis (rather than a diagnosis of exclusion) that should be made by a pediatrician, neurologist, neuropsychiatrist, family doctor, or other physician. “[C]linical interactions during the assessment process are, in themselves, a potentially valuable therapeutic intervention.”
Wolters Kluwer Health

