Clinical depression is a common psychiatric condition with often devastating consequences. A new study in Biological Psychiatry advances our fundamental understanding of the neural circuitry of depression in the human brain.
Treatment of depression is complicated by the disease’s high heterogeneity and notable complexity. Medication to treat depression is available, but one third of patients do not respond to these first-line drug treatments. Other treatments such as deep brain stimulation (DBS) can provide patients with substantial relief, but previous results have been inconsistent. The development of more personalized treatments and improved outcomes requires a better understanding of the neurophysiological mechanisms of depression.
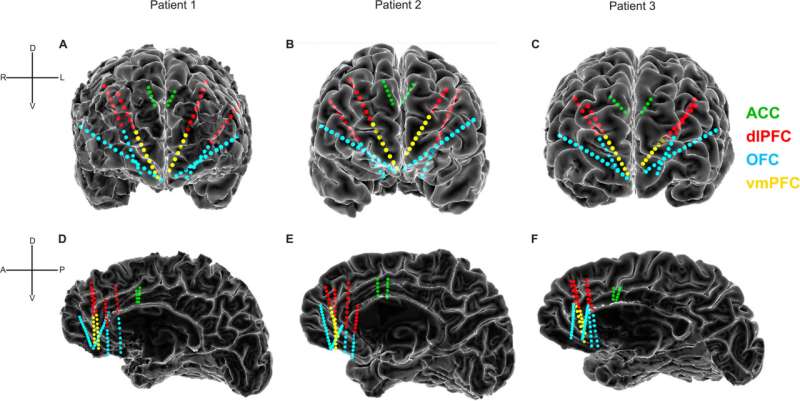
Led by Sameer Sheth, MD, Ph.D., at Baylor College of Medicine, together with Wayne Goodman, MD, and Nader Pouratian, MD, Ph.D., the researchers collected electrophysiological recordings from prefrontal cortical regions in three human subjects, all of whom experienced severe treatment-resistant depression.
The prefrontal cortex plays a significant role in psychiatric and cognitive disorders, influencing one’s ability to set goals and form habits. These highly evolved brain regions are particularly difficult to study in non-human models, so data collected from human brain activity are particularly valuable.
The researchers made electrophysiological recordings of neural activity from the surface of the brain using implanted intracranial electrodes, and they measured each participant’s depression severity for nine days. The patients were undergoing brain surgery as part of a feasibility study for treatment with DBS.
The researchers found that lower depression severity correlated with decreased low-frequency neural activity and increased high-frequency activity. They also found that changes in the anterior cingulate cortex (ACC) served as the best predictive area of depression severity. Beyond the ACC, and in alignment with the diverse nature of the pathways and symptoms of depression, they also identified individual-specific sets of features that successfully predicted severity.
“In order to use neuromodulation techniques to treat complex psychiatric or neurological disorders, we ideally need to understand their underlying neurophysiology,” Dr. Sheth said. “We are thrilled to have made initial progress in understanding how mood is encoded in human prefrontal circuits. As more such data become available, we will hopefully be able to identify which patterns are common across individuals and which are specific. This information will be critical in designing and personalizing next-generation therapies for depression such as DBS.”
John Krystal, MD, Editor of Biological Psychiatry, said of the work, “We now have a growing collection of approaches that can be applied to mapping the circuits and characterizing the neural codes underlying depression. This knowledge will guide next-generation brain stimulation treatments and inform the way we understand and treat depression, broadly.”
Elsevier

