A new technique that combines highly detailed, real-time images of inside the body with a type of infrared light has, for the first time, been used during surgery to differentiate between cancerous tumors and healthy tissue.
The pioneering technique, demonstrated in mice, has been developed by engineers at the Wellcome/EPSRC Centre for Interventional and Surgical Sciences (WEISS) at UCL and surgeons at Great Ormond Street Hospital (GOSH).
Researchers say, the development could have implications for treating neuroblastoma, which is the most common form of solid cancer tumor, other than brain tumors, found in children. Standard treatment typically involves surgery to completely remove cancerous cells, which can be difficult to see as they look similar to the surrounding healthy tissue.
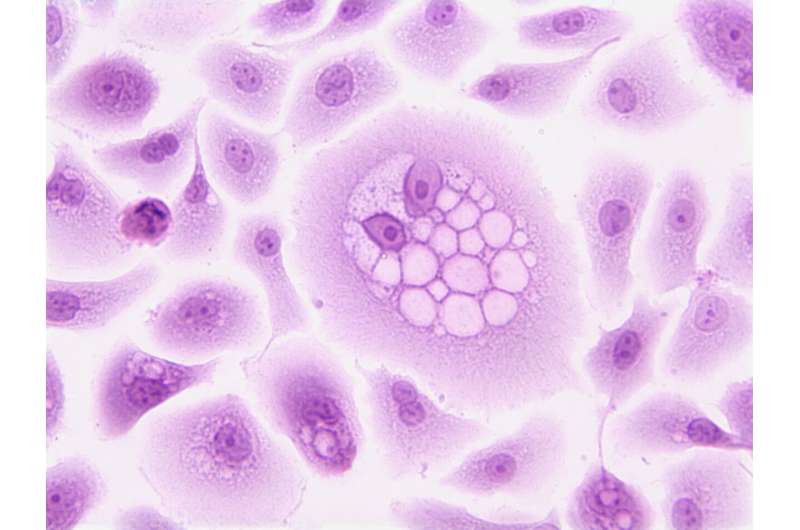
For the study, published in Cancer Research, scientists at UCL and GOSH used a technique called ‘molecular imaging’ during surgery, where chemicals are injected into the bloodstream to act as imaging probes. These chemicals are attracted to cancerous cells in the body, and once attached, the probes light up through a process called ‘fluorescence’, which in turn lights up the tumor. The technique, used during preclinical testing in mice, successfully revealed part of a tumor that had not been removed during surgery.
Next the team wanted to test whether they could improve the visual quality of the images, by using a ‘new’ type of light, short wave infrared light (SWIR), that has only recently become accessible to scientists through new technology.
For this they used a special high definition camera to capture SWIR fluorescence. SWIR is invisible to the naked eye and has a longer wavelength than visible light, allowing it to penetrate deeper into the tissue to provide sharper, more detailed images. Using this technique, surgeons were able to distinguish between cancerous tumors and healthy tissue during the preclinical tests.
Team leader Dr. Stefano Giuliani, Consultant Pediatric Surgeon at Great Ormond Street Hospital and Associate Professor at UCL Great Ormond Street Institute of Child Health, said, “Surgery to remove neuroblastoma requires a delicate balance. Remove too little and the tumor might grow back, but remove too much and the surgeon risks damaging the surrounding blood vessels, nerves and other healthy organs. This technique effectively lights up the tumor, allowing surgeons to remove it with unprecedented precision. We hope to be able to translate this innovative technology into clinical practice at GOSH as soon as possible to benefit the largest number of children with cancerous tumors.”
Neuroblastoma is a devasting childhood cancer and accounts for 8-10% of all childhood cancers and around 15% of childhood deaths from cancer. In around a third of patients the cancer has already spread to other parts of the body at the time of diagnosis, making it harder to treat.
Unlike X-ray or magnetic resonance imaging (MRI), which focus on organs and bones, molecular imaging produces detailed pictures of biological processes, and can be done live during surgery, meaning clinical teams don’t have to wait for biopsy or culture results when screening for diseases. The SWIR enhances the images in real time.
Dr. Dale Waterhouse (Wellcome / EPSRC Centre for Interventional & Surgical Sciences (WEISS) at UCL) said, “This work shows that SWIR imaging, a technology first used for material inspection, can enhance the surgeon’s vision beyond the capabilities of the human eye, allowing more precise tumor surgery. It is very exciting to be part of an interdisciplinary team where surgeons and engineers work together, pioneering cutting-edge technologies that promise to improve the treatment of patients at GOSH.”
Dr. Laura Privitera (UCL Great Ormond Street Institute of Child Health) said, “Pediatric surgical oncology faces an ever-increasing need for novel technologies and devices that can help visualize tumors intraoperatively. By using targeted fluorescence-guided surgery, we demonstrate the possibility of safely and specifically delineating tumor margins, allowing its differentiation from surrounding healthy tissue. Fluorescence-guided surgery is a game-changing innovation that will help surgeons to obtain safer and more complete resection. It is exciting to be part of this project, and I look forward to seeing this technology translated into the clinical environment.”
Scientists at GOSH and UCL WEISS are now working to fast-track the technology into the operating theater at GOSH within the next 12 months to benefit children with cancerous tumors.
University College London

