The mRNA COVID-19 vaccines developed by Pfizer and Moderna continue to save lives. But a new paper published in the journal Vaccines provides evidence that the two vaccines are not equivalent when it comes to protecting older adults against death.
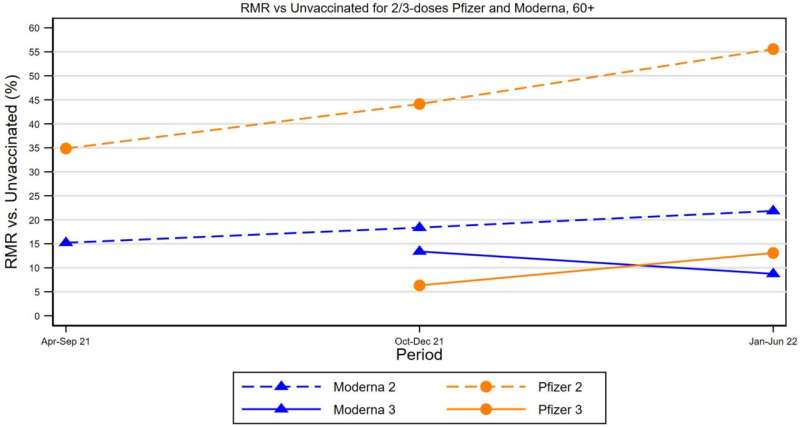
For people ages 60+ who received only the initial two doses, and no booster dose, the risk of death from COVID for Pfizer vaccinees was roughly 2.5 times higher than the risk for Moderna vaccinees. Higher risk was seen throughout the study period, from April 2021 through June 2022. There were no differences in vaccine effectiveness in the 60+ group after a booster dose, and no differences in two-dose effectiveness for younger people.
“We need more refined messaging around boosters that explains who stands to benefit the most, and targets those people,” said senior author Bernard Black, a professor of law at Northwestern’s Pritzker School of Law who specializes in health policy research. He added, “Boosters are crucially important for Pfizer vaccinees. That message needs to be delivered. Our public health agencies should not continue to act as if all COVID vaccines are about the same.”
The study, which measured vaccine protection against death (not hospitalization or other outcomes), also highlights important selection effects: People who got vaccinated were healthier than people who remained unvaccinated. As a group, they were less likely to die for other reasons, and thus less likely to die of COVID even had they not been vaccinated. Moreover, among people who were vaccinated, Pfizer vaccinees aged 60+ were healthier than Moderna vaccinees.
Controlling for these selection effects, both vaccines still significantly reduced mortality, but in the omicron period, the remaining mortality risk relative to unvaccinated people was 57% for two-dose Pfizer vaccinees age 60+, while only 23% for Moderna vaccinees.
For example, if an unvaccinated person aged 60+ had a 1% risk of dying of COVID-19 (based on their age, gender, health and other personal characteristics), a similar person who received two Pfizer doses would have an 0.57% chance of death (43% reduction in risk), while a similar person who received two Moderna doses would have a 0.23% chance of dying from COVID (77% reduction in risk).
A booster dose would reduce remaining risk to about 0.1% for both vaccines. Moreover, the difference in effectiveness between Pfizer and Moderna disappeared for booster recipients.
Thus, boosters are important for all people age 60+, but are especially important for Pfizer vaccinees. A possible reason for this difference between vaccines is that the Moderna dose is much higher than the Pfizer dose (100 μg versus 30 μg). Older bodies may need the bigger kick from the larger Moderna dose to prime their immune systems.
For persons aged 18-49, there were almost no deaths among two-dose vaccinees. For persons aged 50-59, there were a meaningful number of deaths, so a booster dose is important, but no evidence of a difference in effectiveness between Pfizer and Moderna.
In sum, booster protection is highly valuable for older people aged 60+, especially Pfizer vaccines; has substantial value for people in their 50s, but has limited value for younger persons, for whom the initial two doses retain strong protective value against death.
In addition to Black, the team included other researchers affiliated with Northwestern University, the Medical College of Wisconsin, and William and Mary. The authors used a dataset of linked mortality and vaccination records for all adults in Milwaukee County, Wisconsin, (adult population 722,000) from Jan. 1, 2021, to June 30, 2022, to conduct their analysis.
Their study is the first to control for the tendency of the people who received the Pfizer vaccine to be healthier than those who received the Moderna vaccine (at least in Milwaukee, the area that the authors studied).
The key metric that the authors studied was how vaccination affects the COVID Excess Mortality Percentage (CEMP)—the percentage increase in mortality risk due to COVID, relative to the risk from other natural causes. CEMP is measured by dividing COVID-19 mortality for a given group by mortality from non-COVID natural causes for the same group.
Northwestern University

