Habits are like shortcuts for our brains. Once we form a habit—say, putting on a seat belt whenever we get into a car—the behavior becomes almost automatic in the right context. But habit formation isn’t always a boon. The same neural circuitry that helps us to buckle up underlies binge eating disorders, according to a new study by Stanford Medicine researchers and collaborators.
Using brain imaging, researchers saw differences in the neural circuitry that promotes habit formation in people with binge eating disorders, which involves consuming excessive amounts of food in a short time period. The differences were more pronounced in those with more severe disorders. The habitual element of these conditions, the researchers say, could be part of the reason they are so hard to treat.
“A habit is a learned association. Maybe initially the behavior started to achieve a goal, but eventually you’ve done it so many times that you do the action without thinking about the outcome,” said Allan Wang, a medical student at the Stanford School of Medicine and lead author of the study, which was published March 29 in Science Translational Medicine.
“We were interested in whether habit formation in the brain might be involved in a complicated behavior like binge eating,” Wang said.
Tracking the habit
Binge eating disorders seem to have the hallmarks of habits. Episodes can be triggered by context, whether external, like the smell of food or an enticing advertisement, or internal, like feelings of sadness or frustration. People with these disorders also report feeling a loss of control over the behavior, which happens in maladaptive habits ranging from nail biting to drug addiction.
It wasn’t known, however, whether these disorders stemmed from the neural circuitry of habits.
To find out, the researchers first analyzed MRI scans from the Human Connectome Project, a large-scale venture, sponsored by the National Institutes of Health, to map the brain circuits that underlie human behaviors. They focused on a region called the striatum, previously implicated in habits, and a particular part of the striatum called the sensorimotor putamen, which connects to brain regions that govern sensation and movement. Based on these connections, they hypothesized that the sensorimotor putamen would be key to habitual behavior.
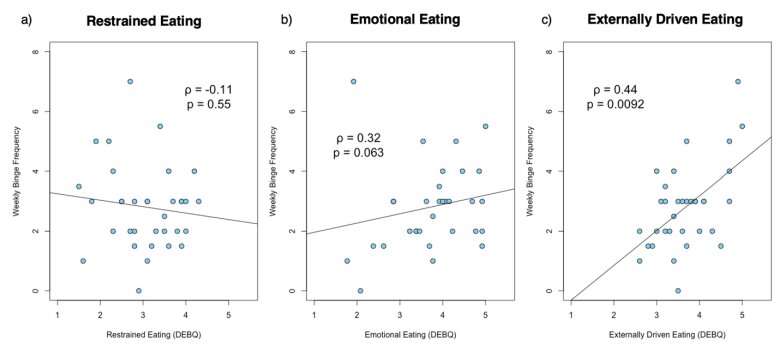
Next, the researchers collected fMRI data, which measures brain activity, from 34 people who had been diagnosed with a binge eating disorder and from 22 healthy controls. All the participants were female. They answered questions about the frequency of their binges and whether they were driven by external or internal factors.
Compared with healthy controls, people with binge eating disorders had notable differences in the sensorimotor putamen’s neuronal connections with several brain regions—confirming the researchers’ hypothesis. They had stronger connections with the motor cortex, which is involved in movement, and the orbitofrontal cortex, involved in evaluating reward value, such as how good a food tastes. They had weaker connections with the anterior cingulate cortex, which regulates self-control.
The extent of the deviations reflected the severity of their disorder, regardless of whether the binges were externally or internally driven.
“Possibly, there’s some loss of self-regulation of this behavior,” Wang said. “At the same time, there’s increased strength of circuits involved in the motor behavior of binge eating.”
Breaking bad habits
Further imaging studies revealed that patients with more altered habit circuitry also had less dopamine binding, or sensitivity to dopamine, in these brain regions. That hints at a mechanism underlying these abnormalities: The sensorimotor putamen uses dopamine, a neurotransmitter, to communicate with the cortex, so changes to dopamine sensitivity can alter these connections, Wang said. And decreased dopamine sensitivity can result from prolonged high levels of dopamine during repeated exposure to rewarding stimuli.
“Our findings suggest that the more dopamine exposure these patients have had in the context of binge eating, the more altered their overall habit circuit connectivity is,” he said.
It’s likely that the habit circuitry is also a factor in addiction and other psychiatric disorders, Wang said. Understanding how neuronal connections go awry in these conditions could guide targeted therapies, such as deep brain stimulation, which uses electric currents applied to the brain to alter neural activity.
“I think there’s also some mental benefit for patients in being able to reframe these behaviors as rooted in habit,” Wang said. “Eating disorders are not a fault of their personality. They’re related to physical changes in the brain.”
Whether people with binge eating disorders are more inclined toward other habits, good or bad, is an open question. “But it’s interesting to think about,” he said.
Nina Bai, Stanford University

