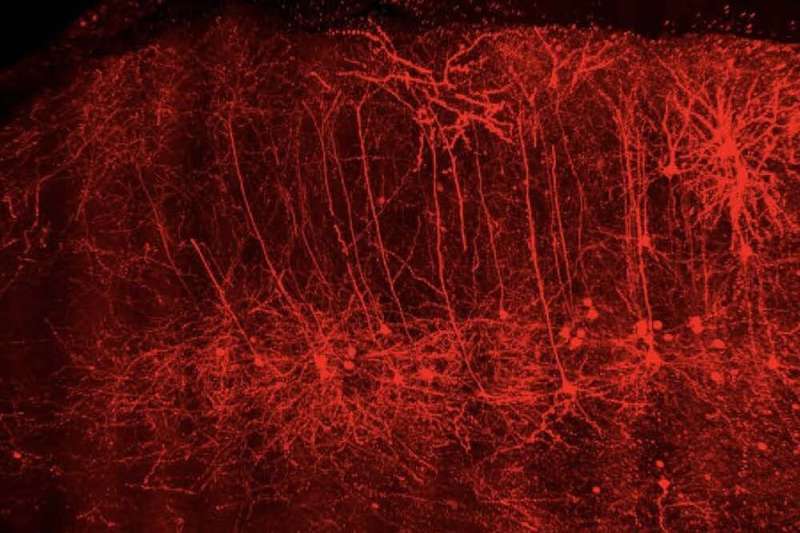
A team of neuroscientists at the Medical University of South Carolina (MUSC) has identified changes in the activity of brain cells known as pyramidal neurons, which contribute to drug seeking in a preclinical model of opioid use disorder. After access to heroin was stopped, these neurons became more excitable. The activity of these neurons was restored to normal by blocking the enzyme protein kinase A (PKA). Inhibiting this enzyme also reduced opioid-seeking behavior. Jacqueline McGinty, Ph.D., professor of neuroscience, and Saurabh Kokane, Ph.D., a postdoctoral scholar in McGinty’s laboratory, recently published their team’s findings in the Journal of Neuroscience.
The risk of opioid overdose can increase upon return to drug seeking and use, or relapse, after a period of not using the drug, or abstinence.
“Prevention of return to use is the key in successful development of effective treatments for substance use disorders,” said Kokane.
“After decades of research on opioid use disorder, three FDA-approved drugs exist, but they only reduce the severity of detoxification symptoms and don’t stop return to use. So, there is a definite need for more treatment options,” he said. “Currently, we lack a comprehensive understanding of the effects of opioids, like heroin, on the neurons that drive return to use. Better understanding these changes may lead to additional treatment options.”
The McGinty Lab at MUSC identified specific types of pyramidal neurons that contribute to relapse. They found that these neurons in a specific brain region, the prelimbic prefrontal cortex, undergo molecular and functional changes during abstinence from heroin, a commonly used opioid, which disrupt its function. The prelimbic cortex is one of the areas of the brain involved in decision-making and behavioral control. Opioids can disrupt normal function in this part of the brain, and in someone with opioid use disorder, this interference can lead to compulsive drug seeking.
Importantly, in this preclinical study, the researchers show that restoration of normal function to these neurons by inhibiting a key enzyme during heroin abstinence can prevent drug seeking in a rodent model.
Understanding relapse
Substance use disorders are chronic, treatable conditions from which people can recover. These disorders are defined in part by the continued use of substances, despite negative consequences, as well as periods of abstinence followed by a return to use, or relapse.
One type, cue-induced relapse, can occur when someone with a substance use disorder encounters a “cue” or “trigger” that may lead that individual to crave the use of a drug. For example, someone with an alcohol use disorder may crave a drink when he or she hears the pop of a champagne cork, or a person with an opioid use disorder may crave heroin if he or she sees drug use on TV.
“These overwhelming cravings may lead those with opioid use disorders to return to use, even if they do not want to,” said Kokane.
“The challenges with compulsive drug use are the loss of the ability to decide between different behavioral options and the lack of resistance to environmental stimuli that remind you of taking an opioid like heroin,” McGinty said.
Losing control
Changes in several brain regions are responsible for cue-induced relapse and make it difficult for a person with substance use disorder to control drug cravings. In this study, Kokane and the McGinty Lab focused on two of these regions: the nucleus accumbens and the prelimbic cortex.
“The nucleus accumbens is a brain area that receives input from the prelimbic cortex and from dopamine-releasing pathways that cause the desire to take the substance again that is associated with all addictive drugs, including opioids,” explained Kokane. During abstinence, aberrant functioning of these pathways is a major contributor to cue-induced relapse.
Generally, the prelimbic cortex and other cortical regions are responsible for deciding whether to act on a feeling or desire. Through its connections with the nucleus accumbens, the prelimbic cortex either motivates us to stop from acting or pushes us to act, said Kokane.
Unique changes in the function of these brain regions caused by opioids make stopping opioid use much more difficult.
“The changes in the brain of someone recovering from substance use disorder drive a return to use when environmental drug cues become overwhelming, but the exact types of changes that occur have not been fully studied,” said McGinty.
Using a rodent model, the MUSC team found that neurons connecting the prelimbic cortex to the nucleus accumbens increase their activity during periods of abstinence from heroin. Rather than putting on the brakes, the increased activity of these neurons may help the nucleus accumbens to drive relapse.
Drug use may then continue uncontrolled, often despite negative social and psychological consequences.
Restoring control
Kokane and McGinty believe that restoring normal activity in the neurons of the prelimbic cortex may prevent cue-induced relapse, but more research is needed.
“We need to understand the changes that occur in neurons during abstinence from heroin in more detail and determine how they lead to relapse,” Kokane said.
The MUSC study also found that an enzyme, PKA, is more active during heroin abstinence. In the prelimbic cortex, where abstinence increased neuronal activity, researchers found that blocking PKA locally returned neuronal activity to normal levels.
This finding led to a new idea for the MUSC researchers: Perhaps PKA inhibition could restore control.
“When we infused the PKA inhibitor into the prelimbic cortex during heroin abstinence, we saw a decrease in cue-induced relapse,” said Kokane.
By blocking PKA, the researchers have discovered one way to restore control to the prelimbic cortex during abstinence from opioids in a rodent model. Importantly, reestablishing control within the brain also led to better behavioral control because heroin seeking was lowered.
“Our findings provide a novel molecular target for the development of future pharmacotherapies,” Kokane said. “We are at a very early stage in this research, but it has potential. Our findings suggest that research should be geared toward developing pharmacotherapies that specifically target functional changes that develop during heroin abstinence in particular types of neurons, like those we identified in the prelimbic cortex.”
Until then, the team is excited to continue its preclinical research to shed light on prelimbic control over opioid seeking and relapse and to uncover additional targets.
“It is important to realize that the brain is constantly adapting to the environment, and that the changes we have documented in the prefrontal cortex during heroin abstinence, while persistent, are not necessarily permanent and are subject to reversal,” said McGinty.
Jordan Carter, Medical University of South Carolina

