Two landmark studies from an international research team have shed new light on antibiotic overuse in newborns, emphasizing the need for better practices and interventions to minimize potential harm to babies’ developing microbiomes and future risks to their health.
The first study, published in JAMA Network Open, presented findings from the largest cohort to date, involving 760,000 infants, looking at the incidence of the severe bacterial infection neonatal sepsis in the first week of life and the corresponding use of antibiotics.
Clinical Professor at The University of Western Australia Medical School Tobias Strunk, who is Program Head of Neonatal and Life Course Health at Telethon Kids Institute and a Consultant Neonatologist at King Edward Memorial Hospital, was a senior author and the sole Australian researcher on the team, and said the study revealed significant overuse of antibiotics in the early stages of life, with Australia experiencing particularly high rates.
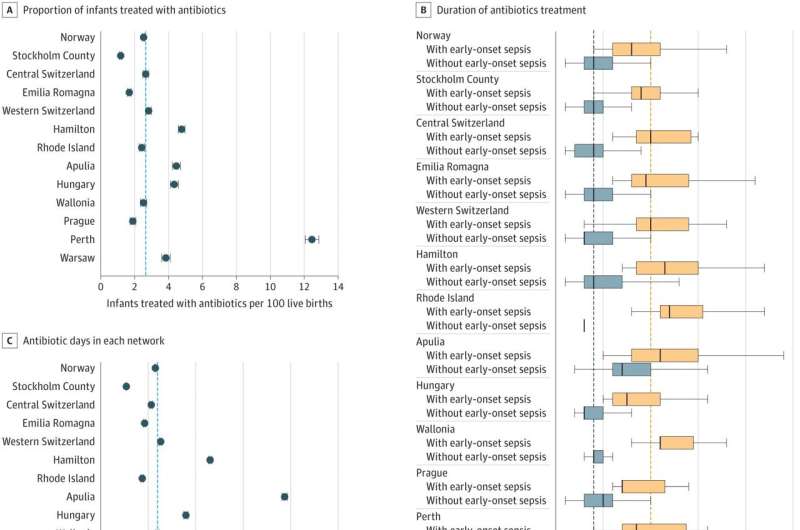
“We found that during the study period nearly three percent of newborn babies received antibiotics in their first week, resulting in an average of 135 days of antibiotic exposure per 1,000 births,” he said.
“Multiple babies—up to 58—were treated with antibiotics as a precautionary measure when one case of sepsis was identified, with a total of 273 cumulative days of antibiotic treatment across all the babies involved in the study.”
The second paper, published in Nature Communications, on which Professor Strunk was also a senior author, provided a more detailed exploration of facts contributing to the overtreatment, the potential adverse effects, and the tools that should be developed and implemented to address and reduce it.
“We found that early-life antibiotic exposure can not only lead to rising rates of antimicrobial resistance but also disrupted the developing microbiome, potentially contributing to various diseases in later life such as diabetes, obesity, inflammatory bowel disease, asthma, and allergies,” Professor Strunk said.
“Neonatal antibiotic treatments were linked to mother-newborn separation, longer hospital stays, decreased breastfeeding rates, and increased healthcare expenses.”
The researchers found a collaborative effort was necessary to optimize the decision-making process surrounding antibiotic therapy in newborns, with three steps proposed to enable this.
“The first was to quantify and share performance data, to create a sense of urgency for behavior change and enable responsible decision-making; and the second to establish an open-access benchmark dashboard comparing the burden of disease with the burden of treatment,” Professor Strunk said.
“The third was to develop educational interventions and innovative techniques, such as leveraging artificial intelligence and routine data analysis, with the ultimate aim to preserve newborns’ microbiomes, combat antimicrobial resistance and improve health outcomes for future generations.”
by University of Western Australia

