Research on the effects of prenatal exposure to the Zika virus has yielded an unexpected dividend: a potentially promising way to trigger natural killer (NK) cells to fight cancer.
NK cells are first-responder immune cells. When enough of their activating receptors are triggered, they mobilize to kill infected, stressed, or cancerous cells at an early stage, before T-cell responses kick in. Most of the triggers for these activating receptors have been a mystery, hampering efforts to exploit NK cells therapeutically.
But a new study published April 5 in Nature may provide an opening.
“There has been a lot of effort to activate NK cells or engineer them for cancer immunotherapy,” says Judy Lieberman, MD, Ph.D., in the Program for Cellular and Molecular Medicine (PCMM), who co-led the study with Caroline Junqueira, Ph.D., in her lab. “We discovered what activates probably the most important receptor on NK cells—something researchers have tried to do for decades.”

From Zika to cancer
The Lieberman lab got a big hint while investigating a seemingly unrelated topic: immune defenses in pregnancy.
In 2020, they showed how NK cells on the mother’s side of the placenta are able to fight some infections without injuring fetal tissues, thereby avoiding a miscarriage.
Then, in 2021, they showed that prenatal Zika virus infection, which can cause severe birth defects, was an exception: Maternal NK cells in the placenta killed Zika-infected fetal cells.
Zika infection of placental cells, they found, causes stress in the endoplasmic reticulum (ER), the part of the cell where proteins are synthesized. The virus reproduces in the ER, overwhelming the ER’s ability to properly fold the newly made proteins. This ER stress activates NK cells to kill the infected cells—specifically by activating a receptor called NKp46.
NKp46 is one of the most important activating receptors on NK cells. It was the first to appear in evolution and is found on all NK cells across species. Past studies have shown that when it’s knocked out in the lab, NK cell action against infections and cancer and immune protection dramatically decline.
But what triggers NKp46 to activate killing? While triggers are known for certain infections, including the flu virus, the specific molecular trigger in other infected cells and in cancer cells has been a mystery.
In the new study, Sumit Sen Santara, Ph.D., and Dian-Jang Lee, Ph.D., in Lieberman’s lab found an answer. They performed an assay to find proteins that bind to NKp46, and a protein called calreticulin was the dominant protein to emerge.
Calreticulin: Harnessing a distress signal
Calreticulin is a “chaperone” molecule in the ER that ensures that proteins are folded properly. During ER stress it goes to the surface of the cell—apparently as a distress signal. NKp46 then recognizes it, enabling NK cells to kill the distressed cell.
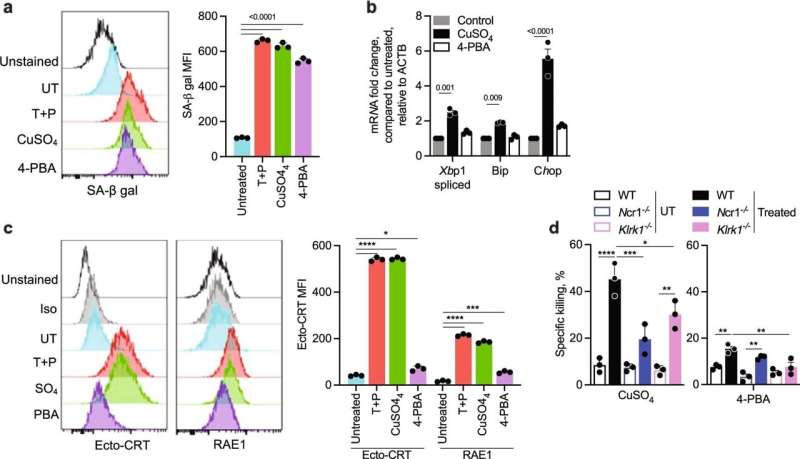
Crucially, when Santara, Lee, and colleagues suppressed calreticulin, knocked it out genetically, or blocked it with antibodies, killing by NK cells was inhibited in mouse tumor models. The same was true in models of aging cells, cells treated with some cancer drugs, and Zika-infected cells. When the team engineered cells to expose calreticulin on their surface, killing by NK cells increased and tumor growth was greatly reduced.
“The best way of manipulating calreticulin therapeutically is unclear, but if we can target it, we can harness NK cells to control a tumor,” says Lieberman. Her lab is just beginning to explore ways that this discovery might be exploited to improve cancer immunotherapy.
Nancy Fliesler, Children’s Hospital Boston

