A Harvard-led study has identified genetic markers associated with preeclampsia and gestational hypertension in a large cohort study. In the paper, “Polygenic prediction of preeclampsia and gestational hypertension,” published in Nature Medicine, the researchers detail how these genetic markers could be used as a predictive risk assessment and offers mechanistic insights into pregnancy disorders.
Preeclampsia and gestational hypertension are common pregnancy complications associated with adverse outcomes, including substantial morbidity and mortality for both mother and child. Current tools for prediction, prevention and treatment are limited.
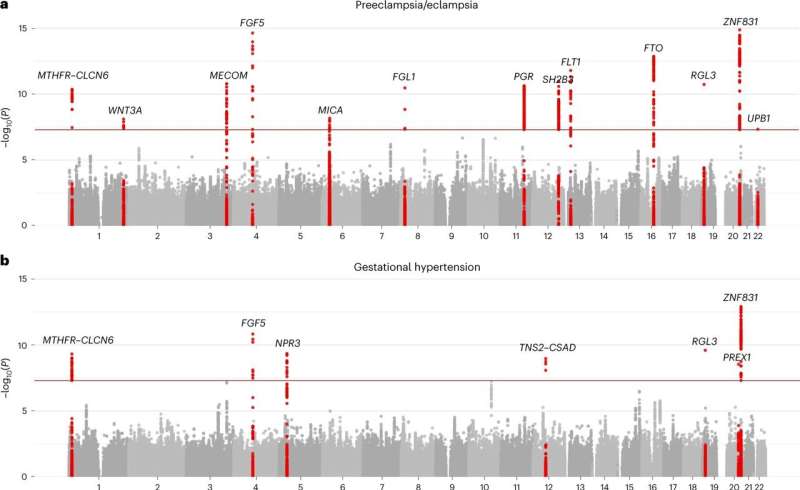
The team examined the associations of maternal DNA variants in 20,064 preeclampsia cases compared to 703,117 control individuals and gestational hypertension in 11,027 cases compared with 412,788 controls. Polygenic risk scores were tuned to a UK Biobank and then tested against other data sets for validation.
The analysis identified 18 independent loci associated with preeclampsia and gestational hypertension, 12 of which were previously unknown, and an additional two genes were implicated in a follow-up meta-analysis. The genes associated highlight potential roles of natriuretic peptide signaling, angiogenesis, renal glomerular function, trophoblast development and immune dysregulation.
Interestingly, almost none of the associated genes reside on the same chromosome, making them less likely to be inherited together.
Low-dose aspirin starting after week 12 gestation is an evidence-based but underused strategy to reduce risk of preeclampsia. To probe the potential clinical impact of incorporating PRS to guide aspirin allocation, researchers examined aspirin eligibility according to current US Preventive Service Task Force major criteria. Those with polygenic risk scores in the top 10% were shown to increase identification as low-dose aspirin-eligible by 30.4%, offering a potential preemptive intervention.
The lead risk variant at the MTHFR–CLCN6 locus has been previously associated with reduced levels of circulating N-terminal pro-BNP43. A recent analysis found that first-trimester levels of N-terminal pro-BNP were unexpectedly lower among female individuals who subsequently developed hypertensive disorders of pregnancy later in pregnancy. These findings suggest that genetic network-driven deficiency in endogenous natriuretic peptide signaling may predispose individuals to hypertensive disorders of pregnancy.
Synthetic natriuretic peptides have been developed, and the authors suggest that natriuretic peptides may represent a future therapeutic target for direct or indirect modulation toward hypertensive disorders of pregnancy prevention and treatment.
Justin Jackson , Medical Xpress

