Until now, scientific evidence has been inconclusive regarding the ability of SARS-CoV-2, the virus that causes COVID, to replicate in the human placenta. Answering this question, as well as understanding the response of the placenta to other viral infections during pregnancy, is crucial for the development of effective preventive and therapeutic strategies for both the mother and the baby.
At Baylor College of Medicine and Texas Children’s Hospital, researchers have taken a novel approach to shed light on the interactions between viruses and the human placenta. They developed a high-resolution map visualizing an array of different immune microenvironments in healthy placentas from uninfected pregnancies, and those from pregnancies affected by COVID infections.
Using this map, they discovered that in many confirmed maternal COVID infections the virus was detected in the placenta at various levels.
In other confirmed cases, evidence of viral replication in the placenta was not found. They also discovered a variety of simultaneous immune responses in niches in the placenta, including both anti-inflammatory niches where replication of the virus was evidently well controlled, as well as pro-inflammatory locations with concomitant viral persistence, including several instances with significant tissue damage to the placenta. Their study appears in the journal Med.
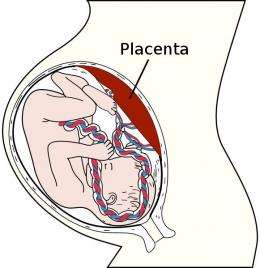
“Previously, it has not been well appreciated that the human placenta comprises a relatively more diverse variety of cell types, including immune cells,” said first author Dr. Enrico Barrozo, a postdoctoral associate of obstetrics and gynecology in Dr. Kjersti M. Aagaard’s lab. “The main goal of our study was to investigate how these immune cells organize themselves in microniches of the placenta, an important first step to understanding the interactions occurring between a virus and the cells of the placenta.”
Their approach of using pioneering technologies such as “spatial transcriptomics” allows them and other pregnancy researchers to start to understand how sometimes (but not always) the immune cells of the placenta succeed at controlling viral growth, and in other rare occasions the virus gets the upper hand. They began by creating a detailed catalog of the cell types in the placenta (called a spatial transcriptomic map), which shows their locations of active gene expression in the niches in the placenta’s microarchitecture.
The team of researchers led by Aagaard generated a high-resolution placental map using single-cell, single-nuclei and spatial transcriptomics in coordinated analyses that revealed dynamic immune microenvironments in healthy placentas.
With the map in hand, the team then analyzed placentas of COVID-positive mothers and found evidence supporting three possible outcomes of the infection.
First, they identified cases in which the COVID virus was not found in the placenta, suggesting that the virus was cleared before infiltrating it. Second, in other cases sparse levels of the virus were present in the placenta and associated with little viral proliferation, an anti-inflammatory response and limited proinflammatory outcomes. Third, in rare cases the virus proliferated extensively within niches that also presented hallmarks of a marked pro-inflammatory immune response and tissue damage.
“Based on this exciting work spearheaded by Barrozo, we propose that, in most cases, the placenta likely responds to COVID and other viruses by limiting replication in these small niches of immune microenvironments. By limiting the immune responses to such a micro-local level, these placental microenvironments can sequester inflammatory signaling and limit collateral damage to adjacent and uninfected placental cells,” said Aagaard, the Henry and Emma Meyer Chair in Obstetrics and Gynecology, and professor of molecular and human genetics, molecular and cell biology and molecular physiology and biophysics at Baylor.
“Thankfully, we know that the most common outcome of any viral infection during pregnancy, including COVID, is a healthy mom and an uninfected baby. It would appear that, most of the time, that placental microarchitectural balance between pro-inflammation and anti-inflammation is evenly keeled. However, previous work from our team has shown that severe cases and death can occur with COVID and other maternal infections, and should not be underestimated or trivialized.”
“We want to understand the role of these microarchitectural niches in arming the placenta for protection of that pregnancy, as well as equipping the baby with an active immune system and ability to survive in the COVID world it is about to be born into,” Barrozo said.
Aagaard added, “We like to think of it as a ‘womb with a view,’ or a way for the mom to equip her developing baby to be born into the world with an immune system tailored to fight viruses it is likely to be exposed to after birth.”
Baylor College of Medicine

