McMaster researchers have uncovered a fast and effective way to detect cancer stem cells before the disease recurs in adults who previously underwent treatment.
Mick Bhatia, a professor in the department of Biochemistry and Biomedical Sciences, led the new study, published in Cell Reports Medicine.
Many cases of cancer recur in the body within a few years of previous treatment. While current methods can monitor for tumors that have returned, technology had not yet advanced enough to catch “undetectable” cancer cells that lead to a tumor coming back. Bhatia’s research with adults who previously underwent treatment for acute myeloid leukemia (AML) is a major step forward
Bhatia spoke about the promise of this new detection method and what this means for the future of cancer treatment.
What is the new method that can detect cancer stem cells before the AML returns?
Our detection method is the same one used to detect rare blood stem cells (progenitors) to help determine the quality of donor cells for bone marrow transplants. This measurement has now been applied to AML patients, and we saw that these progenitor cells have the genetic mutations of a specific patient’s disease, which we call leukemic progenitor cells (LPCs).
The detection of these LPCs can predict short and long-term patient survival outcomes, as well if not better than previous measures used in either the clinic or labs for measuring CSCs. Our method has been applied to a large patient sample size of more than 100 AML patients with success.
How might this method be applied in the future to other types of cancers, including solid cell types?
For other types of leukemia such as lymphoid, we reckon a similar progenitor test could be used. We imagine this would be possible for solid tumors, but a new testing method will be needed as each tumor type is different. For example, breast tissue samples will be needed to detect breast CSCs.
We are excited about solid tumor researchers using this paradigm of “progenitors” measured in a dish to predict patient outcomes as we have now established for adult AML disease.
How might identifying and tracking cancer stem cells lead to new or modified treatments, ideally before the disease reemerges?
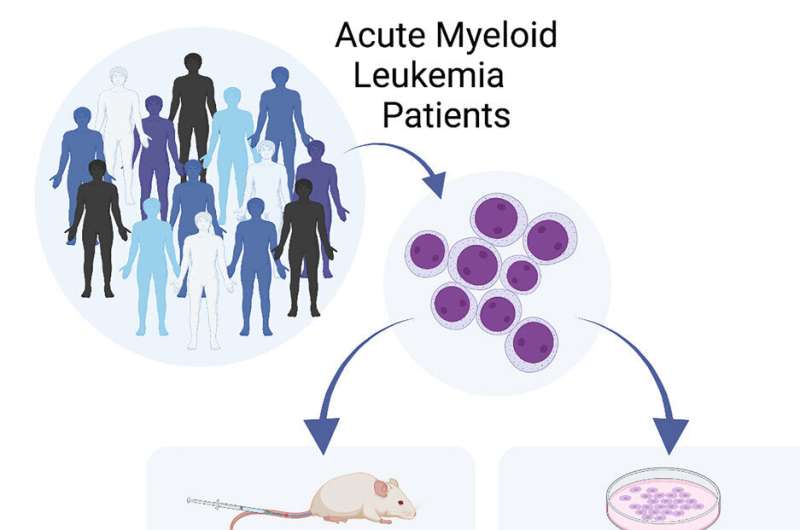
Currently for AML, LPCs are measured using either complex and expensive gene profiles or transplant testing where AML cells would be injected into immune-deficient mice and measured over months with numerous secondary tests being required for this measure of CSCs.
Our method can be adopted by most labs easily, and is relatively inexpensive, takes only eight days and costs only a few hundred dollars. This means might be able to even measure LPCs during and after treatment to predict how well the drugs are working, and the likelihood of the cancer coming back.
This will allow us to dynamically change treatments and monitor patients before the disease gets out of control. This will improve patients’ outcomes by treating with the best drugs based on LPC results, at the right times during therapy. That is our hope and is something we are exploring currently with the LPC in hand. We can see many labs joining a larger collaborative effort as more groups will be able to easily measure these cells and join this effort to better manage our patients.
If I were a cancer patient or their loved one, what would be the key takeaway you would want me to know?
We can measure these rare cells that we think are responsible for disease regeneration—that is, cancer coming back. This will allow us to explore if measuring these cells will allow us to detect disease, treat earlier and/or change treatment during management to better kill these cells in the hope of vastly improving survival rates and reducing the harmful side effects of chemotherapy.
Speaking more broadly, what is the most fascinating aspect of your research on cancer and its stem cells?
It is the fact that such a rare and almost undetectable population like CSCs is responsible for starting and regenerating disease after chemotherapy. CSCs share characteristics with normal cells, and thus hide in the patients, so we need to measure their function and we cannot detect them as easily as we can viruses or bacteria.
We are now finally homing in on cheaper and faster ways to detect and understand CSCs, getting us closer to developing therapies to destroy this root cause of cancer and reduce therapy time lengths.
How would you want your cancer research to contribute to public awareness around a condition that will affect up to 50% of Canadians in their lifetimes (and will kill up to 25%?)
People need to understand that although treatment and detection is getting better, we still fail one in four patients. That is not good enough in my view. We can do better, and there are innovative and practical ways we are doing this. We are testing this with human tissue, instead of mice, in which results are harder to predict, and we can move this to patients fast.
We are all still recovering from COVID-19, but cancer never stopped and is on the rise. We need to get back to business on this disease that represents the number one killer in Canada, but we have limited resources and need more support now.
Fram Dinshaw, McMaster University

