Researchers at UT Southwestern Medical Center have identified a novel parameter of T cells that could help oncologists anticipate which patients would be most likely to develop immunotherapy toxicity. The findings, published in the Journal for ImmunoTherapy of Cancer, could lead to improved treatments for a variety of cancers.
Immunotherapy has grown rapidly in recent years as a treatment for a wide range of common cancers. Some patients, however, acquire toxicities known as immune-related adverse events (irAEs), which can affect almost any organ system at any point during or after treatment. In rare cases, they can be fatal.
“The ability to predict which patients may develop significant immunotherapy toxicity would be extremely useful in the selection of patients, treatments, and monitoring,” said David Gerber, M.D., Professor of Internal Medicine in the Division of Hematology and Oncology and in the Peter O’Donnell Jr. School of Public Health at UT Southwestern. “Our metric—which we call the ‘tolerant fraction’—could play a role in making that a reality.”
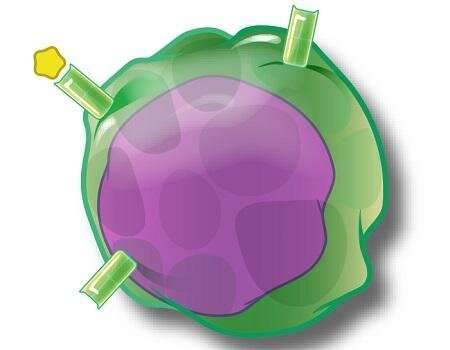
The tolerant fraction represents the proportion of T cells—white blood cells that are primarily responsible for immune responses—not expected to attack normal cells or tissues. To develop and test this parameter, UTSW researchers profiled the receptors of T cells in 77 patients treated with immunotherapy. They also used publicly available data from patients with autoimmune disease and 786 healthy subjects.
“When we compared the new metric to previously studied parameters, the tolerant fraction predicted future immunotherapy toxicity more accurately,” noted Dr. Gerber, who is also a member of UTSW’s Harold C. Simmons Comprehensive Cancer Center. “Patients with a higher percentage of tolerant T cells appear less likely to develop an irAE.”
The team’s findings are preliminary and will need to be confirmed by larger prospective studies, but they hold promise for the development of a novel approach to prevent irAEs.
“Today, immunotherapy toxicities are entirely unpredictable, and there isn’t a clear standard for how to monitor patients for potential irAEs,” Dr. Gerber added. “As a result, some clinicians may be reluctant to use immunotherapy for early-stage cancers or to recommend the most aggressive and potentially toxic treatments, such as combination immunotherapy regimens. The ability to understand a patient’s risk for these toxicities and customize clinical monitoring could lead to more patients receiving more effective treatments more safely.”
UT Southwestern Medical Center

