E. coli is a well-known risk factor in food preparation and hygiene, but how does it cause damage in the body and how does an outbreak have the power to send hundreds to hospital, potentially with kidney damage?
Brian Coombes is professor and chair of the Department of Biochemistry and Biomedical Sciences at McMaster University, and the Canada Research Chair in Infectious Disease Pathogenesis. His lab’s major focus is on drug-resistant bacteria associated with acute and chronic disease.
Coombes, a fellow of the American Academy of Microbiology, shares what you need to know about E. coli and how to prevent it.
What is E. coli?
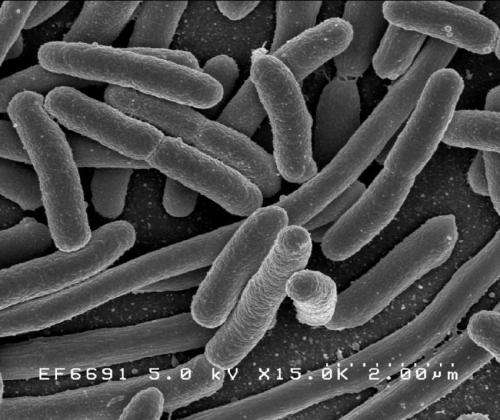
Escherichia coli (or E. coli) is a bacteria that is mainly found in the guts of mammals. In most cases, E. coli do not cause disease in animals and humans, but some strains have evolved to be quite pathogenic to humans. These more dangerous strains are the ones associated with outbreaks and severe disease.
Why does an outbreak cause such severe illness?
Severe illness linked to E. coli is all about the strain involved. Some strains of E. coli are relatively harmless, while others cause serious illness ranging from diarrhea, to bloodstream infections, to organ damage. The strains associated with outbreaks tend to have a very low infectious dose (the minimum number of bacteria you need to ingest in order to become infected) and so even a small number of bacteria can spread to many people relatively easily.
What treatments are available for E. coli infections?
For the E. coli strains linked to the recent outbreak in Alberta, there are few treatment options that target the bacteria directly. Antibiotics can not be used because they make the illness worse by making the bacteria produce more of the toxin that is harming the body. Supportive therapy such as IV fluids and nutrition are used in the hospital setting for these types of infections.
What are some promising advances in treating E. coli infections?
Advances in treating E. coli infections, like the strain causing the outbreak in Alberta (O157:H7), are not that well developed. Phage therapy might be a promising route, and also new treatments that try and block the bacteria from sticking to our cells and treatments that try and inhibit the bacteria’s ability to make toxins.
What are some of the long-term effects of an E. coli infection?
Infections caused by Shiga toxin-producing E. coli can have quite serious short and longer-term effects. In the short term, about 10% of people infected will develop kidney damage associated with the bacteria’s toxin. This condition is called hemolytic uremic syndrome (HUS) and requires dialysis to help the body remove toxins while the kidneys try to recover. In extremely serious cases, the kidneys may sustain permanent damage that limits their function.
These infections have also been associated with increased risk of chronic gut disorders, like irritable bowel syndrome, and disease, like inflammatory bowel disease (ulcerative colitis and Crohn’s disease). This increased risk for IBS and IBD can last for years after the infection first took place.
Who is most at risk?
We generally think that people with less developed or weakened immune systems are most at risk, including children.
How can people protect themselves?
Good personal and food hygiene are required to protect yourself against infection from E. coli. These bacteria can be transmitted to humans in undercooked meat products but have also been associated with uncooked foods, such as raw vegetables that are sometimes fertilized with manure that is contaminated with E. coli. Washing vegetables thoroughly with copious amounts of fresh water is recommended.
Jennifer Stranges, McMaster University

