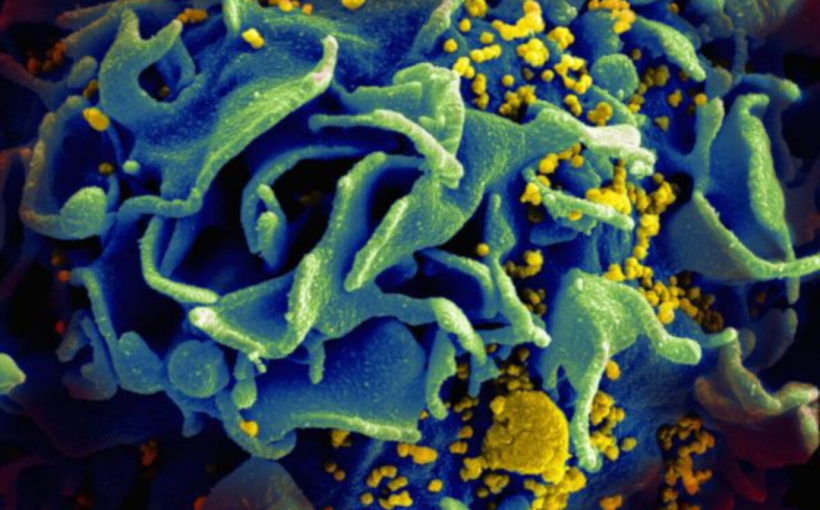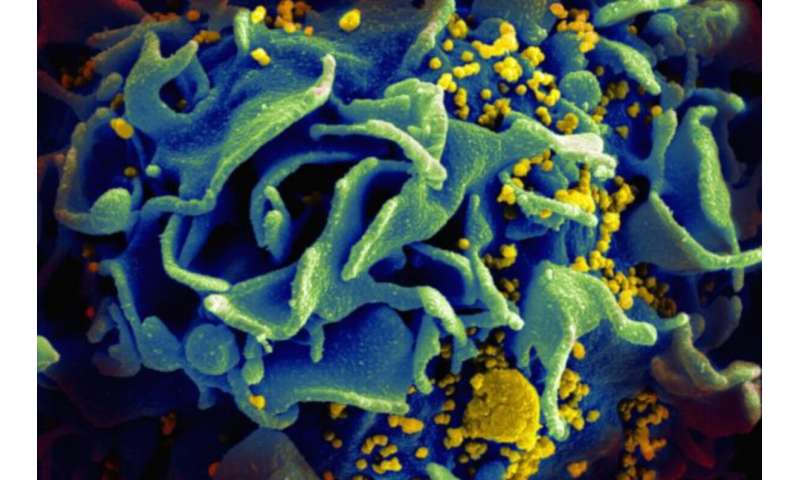
The major obstacle to curing HIV is a vast reservoir of “latent, replication-competent proviruses,” which have infiltrated the very cells that help orchestrate the immune response.
Of all barriers to curing HIV, none pose as difficult a conundrum as latency, a quiescent phase in which proviruses essentially lie in wait, but remain capable of reactivation. A provirus is an inactive virus harbored by a cell. And in the case of HIV, the cells that provide a safe provirus haven are the various subpopulations of CD4+ T cells, key members of the immune system.
In the latent phase, proviruses evade surveillance by the immune system and escape annihilation by antiretroviral drugs. Those two factors alone have made HIV an extraordinary puzzle to solve.
Dr. Robert F. Siliciano, a professor of medicine at Johns Hopkins University, whose research defined the understanding of the HIV reservoir, has been studying the phenomenon for more than two decades.
In the latest research paper published by Siliciano and his collaborators at the University of California, San Francisco, and the Howard Hughes Medical Institute in Baltimore, the team underscored a salient point: Although various CD4+ T cell subpopulations harbor latent proviruses, they show low inducibility of HIV-1 proviruses under experimental conditions. Solving HIV latency ultimately paves the way to a cure, these investigators say.
“Latency may initially be due to the lack of key host factors needed for HIV gene expression,” said Siliciano, who is in the vanguard of researchers who want to eliminate the stubborn reservoirs of HIV proviruses.
Siliciano told Medical Xpress that “over time, epigenetic changes might contribute to further silencing HIV gene expression,” a factor that may drive HIV into a deeper state of latency.
To get a sense of how perplexing this pool of latent proviruses can be, Siliciano’s team emphasizes that antiretroviral therapy can effectively block HIV replication in infected patients, and prevent or reverse immunodeficiency among those who faithfully take their medications. But viral replication resumes within weeks after treatment is interrupted, and the bombardment of the body by newly replicating viruses arises from the pool of latent HIV proviruses, sleeper pathogens that reactivate to perpetuate infection.
Writing in Science Translational Medicine, Siliciano and his colleagues noted that research has shown that proliferation of HIV-infected CD4+T cells constitutes “a major factor in the generation and persistence of the latent reservoir.”
Intact HIV-1 proviruses, Siliciano and his colleagues found, are similarly distributed across different memory CD4+ T cell subsets. In their research, the team studied latency as it related to central memory T cells, transitional memory T cells, and effector memory T cells.
For the past 40 years, the global HIV/AIDS pandemic has been a major public health concern. The infection is caused by a retrovirus, an RNA pathogen that has an enzyme—reverse transcriptase—that uniquely allows the transcription of viral RNA into DNA upon entering the host’s cells. HIV’s DNA then can insinuate itself into the chromosomal DNA of the host, where viral is expressed.
Since the HIV/AIDS pandemic began in the early 1980s, an estimated 75 million people have been infected with the virus, and approximately 32 million have died, according to the World Health Organization. Antiretroviral drugs can control infection but they are not cures because of the powerful phenomenon of viral latency.
Yet, other viruses are more dependent on latency as a survival mechanism than HIV, which uses it in addition to a ability to replicate at an alarming rate.
“For some viruses, especially those of the herpes virus family, latency is a key viral strategy to avoid the immune response. HIV avoids the immune response by rapid evolution and replicates continuously in untreated people,” Siliciano said. “Latency occurs when some activated T cells become infected as they are reverting back to a resting state in which host factors needed for HIV gene expression are no longer available.”
Research aimed at curing the infection is continuing despite a major recent setback to produce an HIV vaccine, which scientists had hoped might prevent infection altogether. A clinical study based in South Africa known interchangeably as the HVTN 702 or Uhambo trial, was canceled by the National Institute of Allergy and Infectious Diseases in the United States, the study’s sponsor.
Siliciano and his collaborators, meanwhile, titled their research paper “Different Human Resting Memory CD4+ T cell Subsets Show Similar Low Inducibility of Latent HIV-1 Proviruses.” Experimentally, they examined subpopulations of CD4+ T cells from 10 HIV patients on antiretroviral therapy.
The experimental work was based on this deceptively simple premise: In certain CD4+ memory T cell subsets, the provirus may be in a deeper state of latency, allowing the cell to proliferate without producing viral proteins. This may, in turn, allow the virus to escape immune clearance. To evaluate provirus latency, the team used a multiple stimulation viral outgrowth assay to culture CD4+ T cells.
“The assay is a variation of the one we used initially to discover the latent reservoir,” Siliciano said. “If you activate T cells, then latency can be reversed because the host factors now become available in the nucleus.”
Science Translational Medicine