A patient-specific tumor organoid model is being used to identify the most effective chemotherapy protocol to treat appendix and colon tumors, a personalized medicine approach that is showing promise. The organoids were created by researchers at the Wake Forest Organoid Research Center (WFORCE), a joint effort by the Wake Forest Institute for Regenerative Medicine (WFIRM) and the Wake Forest Comprehensive Cancer Center.
Treatment for advanced stages of colon and appendiceal cancer with spread in the abdomen consists of cytoreductive surgery which removes tumors from the organs in the abdominal area which is then followed by hyperthermic intraperitoneal chemotherapy (HIPEC). As its name suggests, HIPEC is a cancer treatment that involves filling the abdominal cavity with chemotherapy drugs that have been heated at a specific temperature. Paired together, the two treatments increase life expectancy for patients that in the past were deemed candidates only for palliative approaches.
With the patient-specific tumor organoid model, doctors can test the effect of HIPEC on individual tumors to tailor the conditions needed for optimal effect, thus providing a personalized medicine approach for each patient. Appendix cancer is a rare disease and affects only 1 in 100,000 people while as many as 200,000 people in the U.S. are diagnosed each year with colon cancer.
“Patients undergoing the combination of cytoreductive surgery and HIPEC endure a long surgery that lasts for many hours,” said Konstantinos Votanopoulos, MD, Ph.D., professor of surgery and senior author of the study published recently in the journal Annals of Surgical Oncology.
The effect of intraperitoneal chemotherapy on the viability of the tumor of every individual patient is largely unknown, Votanopoulos said. “With this organoid platform we can quantify the impact of each drug in killing cancer cells. We can select the correct drug for the correct patient at the correct concentration and temperature, or even spare the patient from a procedure that will not substantially improve his or her outcomes.”
An important finding of this work is that every tumor responds to heat differently with some tumors having showing dramatic response while others showing minimal or no meaningful response at all. The authors conclude this is probably related to genetically determined biologic machinery built in the cancer cells to counteract the impact of hyperthermia. Votanopoulos said a future hope would be to perform an image guided biopsy and grow organoids that will determine the optimal approach for each patient.
Shay Soker, Ph.D., a co-author and professor of regenerative medicine at WFIRM, said the study suggests that “the organoid model can accurately represent what occurs inside a patient’s body. The research continues to show that organoids are promising candidates for drug screening to assist in clinical decision making as well as in the study of how environmental factors, viruses or toxins impact cellular function of both normal and tumor cells.”
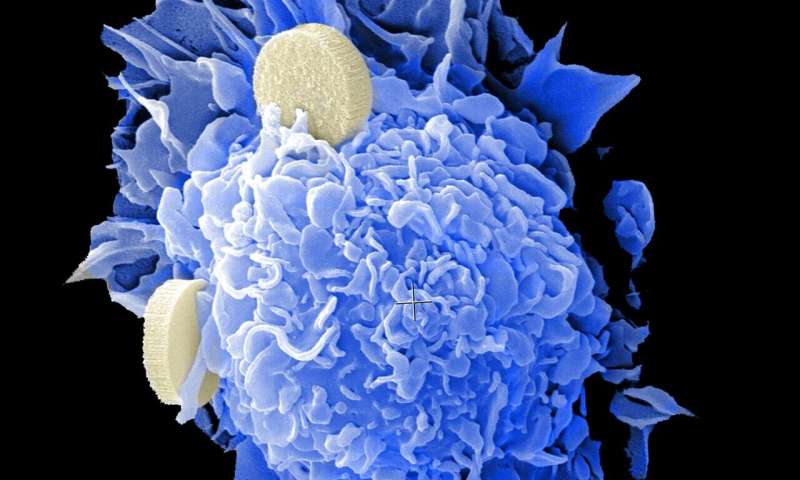
Organoids are tiny, 3-D tissue-like structures created in the laboratory that mimic the function of human tissues and organs such as the heart, liver, lung, blood vessels, as well as cancerous tumors. The organoids are used as a testing and predicting platform to model diseases, evaluate efficacy and/or toxicity of new and existing drugs, and can also be used to test environmental hazards.
“Using a patient-specific tumor organoid model will eventually allow patients to be treated with the best available chemotherapy, while sparing the toxicity of drugs that are not effective for their specific tumor,” said Steven Forsythe, MS, first author of the study.
Wake Forest University Baptist Medical Center

