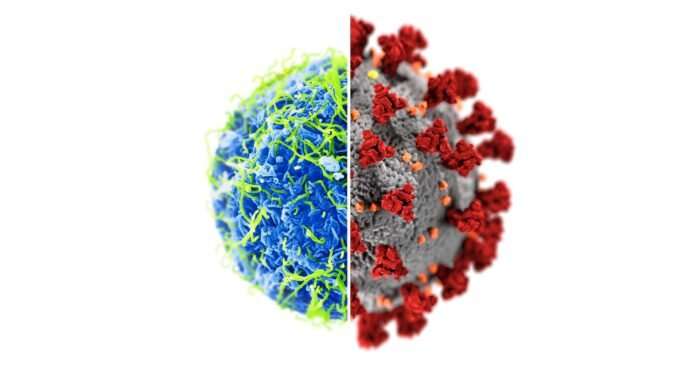
Despite not having safety and efficacy data from the final phase of clinical trials, China and Russia have already started COVID-19 vaccinations and have been widely criticized for prematurely exposing the public to these unlicensed vaccines.
While this approach remains tenuous, it is not unprecedented for countries to issue emergency use authorizations for unlicensed vaccines during public health emergencies. In fact, more countries are expected to issue emergency use authorizations for COVID-19 vaccines in the days and months ahead. And it’s something Canada should not rule out, says Western University’s Maxwell J. Smith. But the key to successful emergency use authorizations is transparency, yet another missed step by China and Russia.
In a new paper published today by The Lancet, Smith and his collaborators from Western’s Faculty of Health Sciences study recent experiences where emergency use authorizations were granted for investigational Ebola vaccines in Guinea and the Democratic Republic of the Congo in order to identify key lessons that should guide emergency use authorizations for COVID-19 vaccine candidates.
“We have to be very transparent about how emergency use authorizations are done,” said Smith, a member of the World Health Organization’s Ethics and COVID-19 Working Group. “We need to make sure decisions are based on favorable risk-benefit ratios. And we need to make sure that exactly what constitutes a favorable benefit–risk ratio is informed by engaging relevant communities.”
Emergency use authorizations are a regulatory mechanism enabling the public to gain access to promising investigational drugs, devices, and vaccines when they have not yet received regulatory approval and licensing.
“We have an ethical imperative to learn from our prior experiences. Countries like Canada, and our regulatory authorities like Health Canada, don’t have a lot of experience issuing emergency use authorizations so we should look to examples where this has been done and try to learn from them,” said Smith, co-director of Western’s HELP (Health Ethics, Law and Policy) Lab.
“COVID-19 is a public health emergency of international concern. And it’s going to need a novel vaccine so it’s pretty similar to the Ebola situation in Africa so we should learn from it,” said Smith. “The other thing is that Guinea and the Democratic Republic of the Congo, which ultimately provided access to unlicensed vaccines, did so in a very transparent and coordinated fashion with the World Health Organization. That stands in stark contrast to what Russia and China have done with their COVID-19 vaccines.”
Smith says that even if China and Russia COVID-19 vaccines are safe and effective, without transparency and rigorous ethical oversight the public may not trust them.
In The Lancet, the Western team of researchers argued that four ethical conditions should be met for emergency use authorizations for COVID-19 vaccines, including public access to evaluation criteria, community engagement, ethical and regulatory oversight and a favorable benefit–risk ratio based on quality, safety, and performance.
“Satisfying these conditions is likely to ensure the scientific and ethical integrity of, and public trust in, emergency use authorizations for COVID-19 vaccines, and mitigate the potentially pernicious influence of national politics on global vaccine efforts,” said Smith.
A leading expert in infectious disease ethics and health equity, Smith is also the co-author of “Fair Allocation of Scarce Medical Resources in the Time of COVID-19,” published earlier this year in The New England Journal of Medicine.
Jeff Renaud, University of Western Ontario

