Every day, ten Americans die from asthma. While quick-acting inhalers and medications can reduce inflammation during an asthma attack, people with asthma have few tools to prevent the next attack from coming.
Now researchers at La Jolla Institute for Immunology (LJI) have discovered that blocking two immune molecules at the same time is key to preventing asthma attacks in a mouse model.
“We have found a way to block the acute asthmatic inflammatory response—and we saw a strong, long-lasting reduction in asthma exacerbations,” says Michael Croft, Ph.D., professor at LJI and senior author of the new study, published November 5, 2020, in The Journal of Allergy and Clinical Immunology.
When a person with allergies encounters an asthma trigger, harmful T cells boost their numbers in the lungs and release molecules that cause inflammation. The new study shows how to throw a wrench in this process.
For the study, the Croft Lab focused on blocking OX40L and CD30L, which are signaling proteins similar to tumor necrosis factor (TNF), a protein that is the target of several FDA approved drugs. These molecules are upregulated by allergens and can activate the harmful T cells that drive inflammation in asthma.
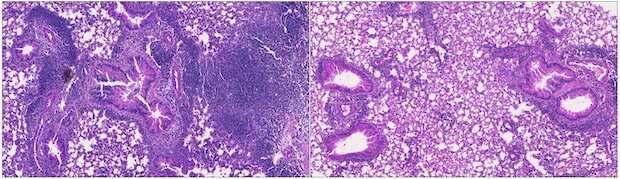
In the new study, Croft and his colleagues worked with a mouse model sensitive to house dust mites—a very common allergy and asthma trigger. The scientists showed that blocking OX40L and CD30L at the same time could stop the expansion and accumulation of harmful T cells in the lungs during an allergen attack, and this then led to reduced inflammation.
“The combination of taking out the two sets of signals allowed for a strong reduction in the number of those pathogenic T cells, whereas only neutralizing either one had a relatively mild effect” says Croft. “That was quite a significant finding.”
Importantly, blocking both OX40L and CD30L also reduced the number of pathogenic T cells that lingered in the lungs following the asthma attack. These “memory” T cells would normally drive inflammation when a person encounters an allergen again. Without OX40L and CD30L on the job, very few of these harmful T cells stuck around in the lungs, and mice had a weaker response to house dust mites for weeks after the initial treatment.
“This suggests we were diminishing the immune memory of the allergen,” Croft says.
This study comes several years after an ineffective clinical trial targeting OX40L. Previous research by the Croft lab and other researchers had suggested that blocking signaling from OX40L could reduce airway inflammation, yet a neutralizing antibody against OX40L did not have a beneficial effect in asthmatic patients with house dust mite or cat allergies.
“Why did it fail?” asks Croft. “The new study supports the idea that simply blocking OX40L was not enough.”
The research sheds light on the complexity of the immune system and suggests that long-lasting therapy of inflammatory and autoimmune diseases may require a multi-pronged targeting approach, especially when trying to limit the number of pathogenic T cells that are the central drivers of these diseases.
A combination therapeutic to block both molecules would be complicated to test (researchers would need to prove the safety of blocking each separately) but Croft thinks either dual antibodies or a “bi-specific” reagent could work to block OX40L and CD30L signaling together in a single treatment.
Croft is now thinking of the next steps for his lab. Blocking OX40L and CD30L reduced memory T cells but didn’t eliminate all of them. Croft thinks additional target molecules could be out there.
“We’re trying to understand what those molecules might be,” says Croft.
La Jolla Institute for Immunology

