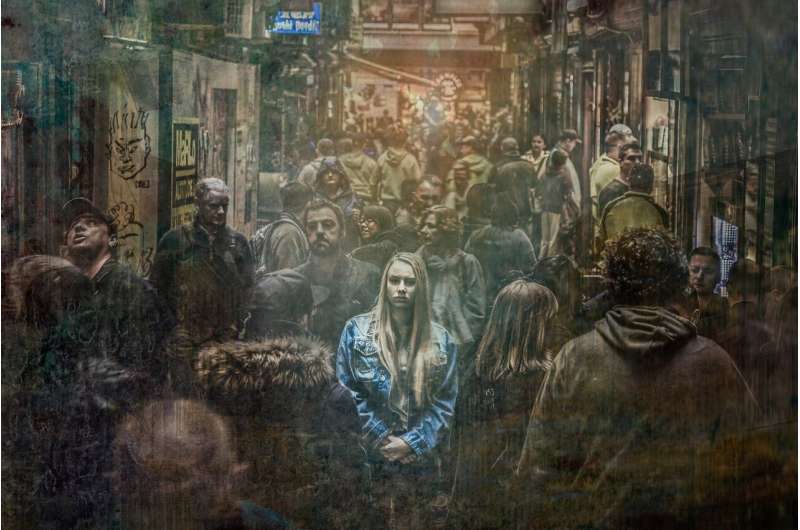
People with lower incomes and who experienced multiple COVID-related stressors were more likely to feel the toll of the pandemic, as the socioeconomic inequities in mental health continue to widen.
Depression among US adults persisted—and worsened—throughout the first year of the COVID-19 pandemic, according to a new study by Boston University School of Public Health (BUSPH).
Published in the journal The Lancet Regional Health—Americas, the first-of-its-kind study found that 32.8% of US adults experienced elevated depressive symptoms in 2021, compared to 27.8% of adults in the early months of the pandemic in 2020, and 8.5% before the pandemic.
The most significant predictors of depressive symptoms during the pandemic were low household income, not being married, and the experience of multiple pandemic-related stressors. The findings underscore the inextricable link between the pandemic and its short and long-term impact on population mental health.
“The sustained high prevalence of depression does not follow patterns after previous traumatic events such as Hurricane Ike and the Ebola outbreak,” says study senior author Dr. Sandro Galea, dean and Robert A. Knox Professor at BUSPH. “Typically, we would expect depression to peak following the traumatic event and then lower over time. Instead, we found that 12 months into the pandemic, levels of depression remained high.”
The study is the first nationally-representative study in the US to examine the change in depression prevalence before and during COVID, using the Patient Health Questionnaire-9 (PHQ 9), the leading self-administered depression screening tool.
The researchers used data from 5,065 respondents to the 2017-2018 National Health and Nutrition Examination Survey (NHANES), as well as from respondents to two COVID-19 Life Stressors Impact on Mental Health and Well-Being (CLIMB) surveys. The first survey included 1,441 respondents and was conducted from March 31 to April 13, 2020, when the majority of the US population was under stay-at-home advisories. The second survey was conducted with the same group one year later, from March 23 to April 19, 2021, and included 1,161 respondents.
Both surveys used the PHQ 9 to assess depression symptoms and gathered the same demographic data, and the CLIMB surveys also gathered data on COVID-related stressors such as job loss, the death of a loved one due to COVID, financial problems, feeling alone, and a lack of childcare.
The survey responses suggested that the burden of depression intensified over the course of the pandemic and disproportionately impacted adults with lower incomes. When adjusting for other demographics, people making less than $20,000 in spring 2020 were 2.3 times more likely to experience elevated depressive symptoms, compared to people making $75,000 or more; by spring 2021, low-income adults were more than 7 times as likely to experience these symptoms.
Although population-level stressors decreased overall during the first year of the pandemic, people experiencing four or more stressors were more likely to also experience elevated depressive symptoms—and least likely to overcome those stressors.
“The sustained and increasing prevalence of elevated depressive symptoms suggests that the burden of the pandemic on mental health has been ongoing—and that it has been unequal,” says study lead author Catherine Ettman, a doctoral candidate at Brown University School of Public Health and chief of staff and director of strategic initiatives in the Office of the Dean at BUSPH. She notes that economic relief and the development of COVID-19 vaccines may have prevented even worse depression outcomes.
“Low-income populations have been disproportionately affected by the pandemic and efforts moving forward should keep this population in mind,” Ettman says. “Addressing stressors such as job loss, challenges accessing childcare, and difficulties paying rent, will help to improve population mental health and reduce inequities that have deepened during the pandemic.”
Boston University School of Medicine

