A cell therapy developed by the executive director of the Smidt Heart Institute stabilizes weakened muscles—including the heart muscle—in Duchenne muscular dystrophy patients, a new study published in the international peer-reviewed journal The Lancet shows.
If the HOPE-2 study’s success is duplicated in the upcoming multicenter, randomized, placebo-controlled HOPE-3 clinical trial, the intravenous cell therapy could become the first Food and Drug Administration-approved treatment for Duchenne patients with advanced disease.
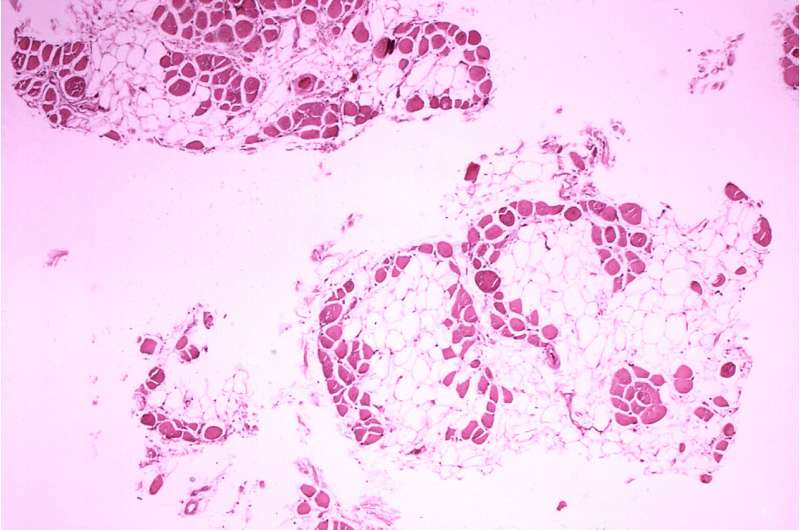
“This therapy is unique in that it addresses two vital needs in patients with Duchenne: physical movement and a healthy heart,” said Eduardo Marbán, MD, Ph.D., executive director of the Smidt Heart Institute at Cedars-Sinai, the Mark S. Siegel Family Foundation Distinguished Professor, an author on the study and the inventor of cardiosphere-derived cells (CDCs), progenitor cells derived from human heart tissue, which have been used in multiple clinical trials.
Duchenne muscular dystrophy is a rare, inherited disorder that mostly affects males. It’s caused by mutations on a gene on the X chromosome that interferes with the production of a protein called dystrophin that muscles need to function. Children born with such mutations have muscle weakness throughout their bodies. This makes it difficult for them to do normal activities like run, jump, climb stairs, stand up after sitting and pedal a bicycle. They can also become extremely sick when muscles in their hearts and respiratory organs weaken.
The prognosis for patients with Duchenne muscular dystrophy is bleak. Most use a wheelchair by the time they are teenagers and don’t typically live into their 30s. There is no cure for the disease. Currently, the only approved medical treatments are aimed at delaying loss of the ability to walk; nothing is available for patients with more advanced disease, who now outnumber those with milder symptoms.
“The HOPE-2 trial is a game changer for muscular dystrophy,” said Craig M. McDonald, MD, the trial’s principal investigator and the professor and chair of physical medicine and rehabilitation and professor of pediatrics, from University of California, Davis Health, one of several sites participating in the trial. “For the first time, we have a treatment which markedly slows loss of arm function and preserves heart function in Duchenne patients. The cells are given intravenously, and only four times a year, so the treatment is not burdensome for patients and their families.”
Other experimental therapies aim to get the body to make dystrophin. The therapy studied in this Phase II clinical trial takes a different approach. It uses heart cells called cardiospheres, or CDCs, which are a type of progenitor cells derived from human heart tissue, to improve the function of skeletal muscle and the heart, at least partly by blunting inflammation. Skeletal muscle mediates voluntary movement, such as that of the arms, while the heart pumps blood throughout the body to sustain life.
“This therapeutic approach makes it possible for everyone with DMD to benefit regardless of their exact genetic mutation, which can vary from child to child,” Marbán said. “The fact that the cells help both heart and skeletal muscle is notable, as no other treatments have done so.”
The trial was sponsored by Capricor Therapeutics, a San Diego- based biotechnology company, which holds a worldwide, exclusive license for this technology and intellectual property and manufactures the cell treatment under the product name of CAP-1002.
“We are extremely encouraged by the results of the HOPE-2 study,” said Linda Marbán, Ph.D., Capricor’s CEO. “We now have conducted HOPE-Duchenne and HOPE-2, the Phase I and Phase II clinical trials using CAP-1002 to treat late-stage DMD patients. These showed statistically significant improvements in upper limb and/or cardiac function in the treatment groups. We are in the process of initiating a Phase III pivotal study, called HOPE-3, which the FDA has signaled as the next step toward product approval for the serious unmet need of DMD.
“https://www.youtube.com/embed/VAvAxL7O1T8?color=white
The study included 20 boys from multiple hospitals across the U.S. All were 10 or older and all had Duchenne muscular dystrophy.
Each patient in the trial had what investigators classified as “moderate upper limb impairment,” meaning their function ranged from being able to raise both arms simultaneously above their heads by flexing at the elbow to being able to raise one or two hands to the mouth, but not bring a cup to it.
“Children with DMD eventually become dependent on their arms for most of their activities, such as eating and operating their wheelchair,” McDonald said. “Any improvement in upper limb function can make a huge difference.”
Eight children were randomly assigned to receive the cell therapy and 12 were randomly assigned to receive the placebo. The cells and placebo were administered intravenously every three months for a year. The study was double-blinded, meaning neither the doctors nor patients knew who was getting the treatment or placebo.
Results showed patients who were given CAP-1002 experienced less loss of ability in their upper limbs after 12 months than patients who received the placebo. Although children given CAP-1002 still lost some upper limb movement during that period, they did so at a rate that was 71% slower than in children who didn’t receive the therapy.
Heart function also improved in children given the cell-based therapy versus the placebo—an important finding since heart failure is a main cause of death in people with Duchenne muscular dystrophy.
The new Lancet study is the latest in Marbán’s body of work that harnesses CDCs to improve heart function. Results from the earlier CADUCEUS trial, published in The Lancet in 2014, showed that infusing CDCs into the hearts of heart attack survivors significantly reduced their heart attack scars. The present study uses intravenous cell delivery, which is much easier than cardiac infusion.
The treatment appears to be safe. One child experienced a severe allergic reaction to CAP-1002 during a second intravenous infusion and required an injection of epinephrine and hospitalization. After that, the investigators put the children on a pre-treatment drug regimen to reduce the risk of allergic reactions. Only one child experienced an allergic reaction after this was implemented, and he did not require medication or hospitalization.
More studies are needed to learn whether the effects of this therapy last longer than 12 months and prolong the lives of children with DMD.
“Here we show the promise of cell therapy in preventing the progression of heart disease in a rare genetic disease, but there is good reason to believe that such therapy may one day be used for more common forms of heart failure,” Marbán said.
Cedars-Sinai Medical Center

