Neutralizing antibody levels against the original COVID-19 virus and omicron variants in vaccinated adults tend to decline by at least 15% per month after a single booster shot, a new study using serum from human blood samples suggests.
Data from two adults in the same study who had a dramatic loss in antibodies but received a second booster showed that the second dose completely restored antibodies to protective levels.
“The message from our study is clear: If you have a dramatic loss of antibodies from the first booster, you definitely need a second booster to get antibodies back,” said Shan-Lu Liu, senior author the study and a virology professor in the Department of Veterinary Biosciences at The Ohio State University.
“It’s not surprising to us to find that we see this antibody decline—in general, vaccine-induced antibodies decline over time regardless of the virus, and especially if the virus changes over time in the way that SARS-CoV-2 has changed,” said Liu, also a professor in the Department of Microbial Infection and Immunity.
The study is published as a letter to the editor today (Sept. 7, 2022) in the New England Journal of Medicine.
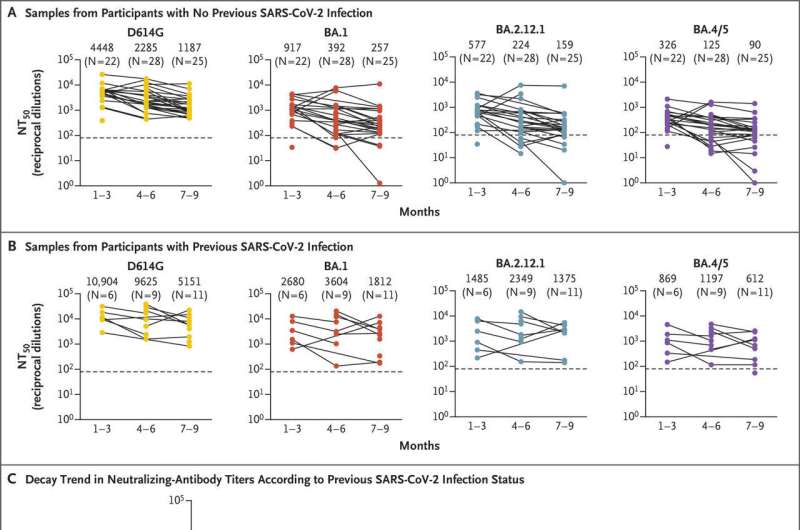
Researchers tested serum from 46 health care professionals who had received the initial two-dose mRNA vaccine course and, later, one booster shot between one and nine months before their antibody levels were tested against the parent SARS-CoV-2 virus and the most dominant omicron variants, including BA.5, among recent and current infections. The team also had access to samples from two vaccinated health care workers who had received the second booster shot.
Using statistical modeling to account for the variable passage of time after the first boosters among the sample population, researchers estimated an average rate of decline in neutralizing antibody levels of nearly 18% against the parent virus, 19.5% against the BA.1 omicron variant, 18.4% against BA.2.12.1 and 19.6% against BA.4/5 every 30 days. Put another way: Neutralizing antibody titers were about 1.7 times higher one to three months after the first booster than the levels detected seven to nine months after the shot, dropping about 50% within 95-108 days.
The declines were slightly less steep in vaccinated health care workers who had also had a COVID-19 infection, but the differences were not significant by statistical standards, said co-first author John Evans, a Ph.D. candidate in Ohio State’s Molecular, Cellular and Developmental Biology Program who works in Liu’s lab.
In fact, the data reinforced the need for booster shots even after a COVID-19 infection: “People with infection got a small antibody benefit from having had the infection,” Evans said. “But overall, there was not much of a difference in the rate of decline across variants.”
“We had two people who had an almost complete loss of neutralizing antibodies against the current predominant BA.5 strain at three to four months following the first booster vaccination but showed a complete recovery of antibody response in the blood after the second booster,” said Panke Qu, the leading co-first author of the study and a Ph.D. candidate in the College of Veterinary Medicine’s Comparative Biomedical Sciences Graduate Program.
Previous work led by this research group showed the importance of a single booster to maintain protection against SARS-CoV-2, and omicron in particular. In a June 30 letter to the New England Journal of Medicine, Liu’s lab reported that the BA.4/5 and BA.2.12.1 omicron subvariants showed substantial resistance to immunity generated by the two-vaccine course compared to the earlier BA.1 and BA.2 subvariants, but that a single booster shot provided sufficient neutralizing antibodies against the two later subvariants three to four weeks after the vaccination. The team also reported in May that a COVID-19 booster shot provided strong and broad antibody protection against the range of omicron sublineage variants that were in circulation at the time.
“Now we’re showing how long the booster can last, which is a very important topic because people have been talking about whether and when to get a second booster,” said Liu, also associate director of Ohio State’s Center for Retrovirus Research and a program co-director of the Viruses and Emerging Pathogens Program in Ohio State’s Infectious Diseases Institute.
The findings on reduced antibody durability from a single booster come a week after the Food and Drug Administration announced approval of an updated booster containing components from the original SARS-CoV-2 strain and the BA.4/5 omicron subvariant.
“Our data tells us the second booster is really important, but of course we could not say anything about the new formulation,” Liu said. “We’re continuing our studies to analyze the neutralizing antibody response and durability of a second booster, including the new formulation.”
The researchers conducted the cell-culture studies using pseudoviruses—a non-infectious viral core decorated with different SARS-CoV-2 spike proteins on the surface structured to match known mutations. The method used to detect neutralizing antibodies in the blood samples accounted for the varying concentrations of antibodies produced by individuals.
Statistical modeling was performed by co-author Lianbo Yu, a biostatistician in biomedical informatics and the Center for Biostatistics in Ohio State’s College of Medicine. Qu conducted most of the experiments in the current study.
Emily Caldwell, The Ohio State University

