HIV anti-retroviral therapy is considered a treatment and not a cure because patients usually carry a reservoir of HIV-infected cells that can re-emerge if treatment stops. These reservoirs have long been thought to be dormant, but two independent groups of researchers report in the journal Cell Host & Microbe on September 13th that a subset of these cells spontaneously produce HIV RNA and proteins that may impact patients’ HIV-specific immune responses.
“It’s a deceptively dormant virus,” says immunovirologist Daniel Kaufmann of the University Hospital of Lausanne, the University of Lausanne, and l’Université de Montréal, who is senior author on one of the papers . “Even in people who are treated, HIV continues to have some activity, and it continues to interact with the immune system. We have to understand if these ongoing interactions have clinically relevant consequences.”
Previous studies have shown that when “dormant” HIV reservoir cells are reactivated in the lab, they produce viral RNA and proteins, but it wasn’t clear whether this phenomenon was happening inside the bodies of people with HIV. “We wanted to understand if this phenomenon is real and, if it is, what parts of the virus are being expressed and do they have an impact on the immune system,” says Kaufmann.
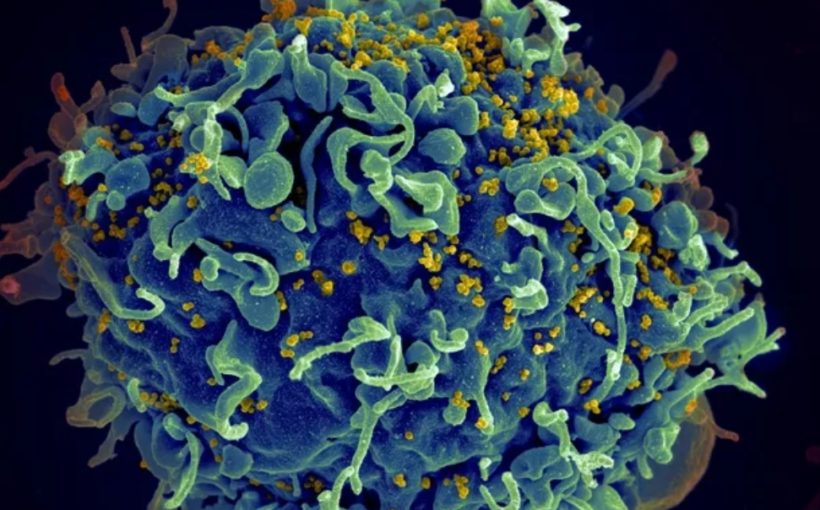
To do this, the researchers took blood samples from 18 people with HIV who had all had been on anti-retrovirals — drugs that block HIV growth without actually killing the virus — for more than 3 years. Then, they used a lab method called RNA flow cytometry to sort CD4+ or “helper” T cells (the type of cell that HIV selectively infects) based on whether they were infected with HIV and, then further, whether they were actively producing HIV RNA or proteins. The researchers also characterized the T cells by role — e.g., whether they were the type of T helper cell that combats intracellular viruses or the type that combats extracellular bacteria — to determine whether any subtypes of CD4+ T cells were more likely to host HIV reservoirs.
“Our technique allows us to look at the individual cells to see if they contain the virus and which parts of the virus they are expressing,” says Mathieu Dubé, an immunovirologist at l’Université de Montréal and first author on the paper led by Kaufmann. “For each patient, we could estimate how many of these cells are still active, and we could also look for associations between viral characteristics and cell characteristics.”
The researchers found that 14 of the 18 patients had HIV reservoirs that spontaneously produced viral RNA. For 7 of the 18 patients, the viral reservoirs also produced viral proteins including p24, a component of HIV’s shell.
“Most of the virus that remains in the body is defective or junk virus that cannot really multiply, but we found these defective viruses can still produce virus RNA and sometimes proteins,” says Kaufmann.
advertisement
Though these pieces of viral RNA and protein were non-functional “debris,” the researchers found that they were enough to stimulate an immune response. Since stronger HIV-specific immune responses were associated with more active HIV reservoirs, the researchers suspect that this immune response may be unhelpful, but more research is needed to test that hypothesis.
“Our data suggest that the RNA and proteins produced by these viral reservoirs could be drivers of inflammation,” says Kaufmann. “This could be important because a subset of the people who are successfully treated with anti-retroviral therapy for HIV still have negative consequences of living with the infection — for example, accelerated cardiac disease, frailty, and premature osteoporosis.”
When they investigated which types of CD4+ T cells were more likely to harbor active viral reservoirs, the researchers found that the active HIV reservoirs were hosted by T cells with a range of phenotypes and functions, though some types did tend to carry more virus than others.
“Some subsets seem to be more prone to hosting viruses, for example, memory cells and Th17 cells that are involved in immune protection in the gut, but there’s no clear, unique type of CD4+ T cell that hosts the virus,” says Dubé. “You can have viruses in most CD4+ T cells.”
Though all the patients in the study were white males, the researchers still observed substantial variation between patients. They say that future studies should further investigate these inter-patient differences and investigate HIV reservoirs in a more diverse suite of patients.
The second paper, led by immunologist Lydie Trautmann at the Vaccine and Gene Therapy Institute of Oregon Health and Science University, also reported that a subset of CD4+ T cells spontaneously express viral RNA during anti-retroviral therapy, specifically in cohorts of Thai participants that initiated therapy at acute versus chronic infection. Fewer viral proteins were seen in patients with acute infection but similar immune responses between both groups were observed.
“Our study suggests that residual immune dysfunction driven by the active HIV reservoir on anti-retroviral therapies could contribute to the lack of viral control after analytical treatment interruption by preventing the differentiation of functional stem-like self-renewing HIV-specific CD8+ T cells that can mount efficient rapid recall responses,” write the authors. “Therefore, HIV remission strategies will likely need to target transcriptionally active proviruses producing viral proteins during anti-retroviral therapies to harness HIV-specific CD8+ T cells to control rebounding of the virus after therapy cessation.”