A phase 1 clinical trial testing a novel vaccine approach to prevent HIV has produced promising results, IAVI and Scripps Research announced today. The vaccine showed success in stimulating production of rare immune cells needed to start the process of generating antibodies against the fast-mutating virus; the targeted response was detected in 97 percent of participants who received the vaccine.
“This study demonstrates proof of principle for a new vaccine concept for HIV, a concept that could be applied to other pathogens, as well,” says William Schief, Ph.D., a professor and immunologist at Scripps Research and executive director of vaccine design at IAVI’s Neutralizing Antibody Center, whose laboratory developed the vaccine. “With our many collaborators on the study team, we showed that vaccines can be designed to stimulate rare immune cells with specific properties, and this targeted stimulation can be very efficient in humans. We believe this approach will be key to making an HIV vaccine and possibly important for making vaccines against other pathogens.”
Schief presented the results on behalf of the study team at the International AIDS Society HIV Research for Prevention (HIVR4P) virtual conference today.
The study sets the stage for additional clinical trials that will seek to refine and extend the approach—with the long-term goal of creating a safe and effective HIV vaccine. As a next step, IAVI and Scripps Research are partnering with the biotechnology company Moderna to develop and test an mRNA-based vaccine that harnesses the approach to produce the same beneficial immune cells. Using mRNA technology could significantly accelerate the pace of HIV vaccine development.
HIV, which affects more than 38 million people globally, is known to be among the most difficult viruses to target with a vaccine, in large part because it constantly evolves into different strains to evade the immune system.
“These exciting findings emerge from remarkably creative, innovative science and are a testament to the research team’s talent, dedication and collaborative spirit, and to the generosity of the trial participants,” says Mark Feinberg, M.D., Ph.D., president and CEO of IAVI. “Given the urgent need for an HIV vaccine to rein in the global epidemic, we think these results will have broad implications for HIV vaccine researchers as they decide which scientific directions to pursue. The collaboration among individuals and institutions that made this important and exceptionally complex clinical trial so successful will be tremendously enabling to accelerate future HIV vaccine research.”
One in a million
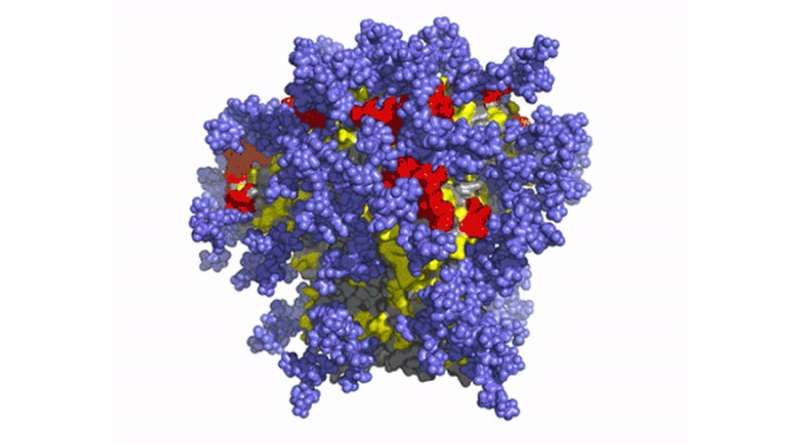
For decades now, HIV researchers have pursued the holy grail of stimulating the immune system to create rare but powerful antibodies that can neutralize diverse strains of HIV. Known as “broadly neutralizing antibodies,” or bnAbs, these specialized blood proteins could attach to HIV spikes, proteins on the virion surface that allow the virus to enter human cells, and disable them via important yet difficult-to-access regions that don’t vary much from strain to strain.
“We and others postulated many years ago that in order to induce bnAbs, you must start the process by triggering the right B cells—cells that have special properties giving them potential to develop into bnAb-secreting cells,” Schief says. “In this trial, the targeted cells were only about one in a million of all naïve B cells. To get the right antibody response, we first need to prime the right B cells. The data from this trial affirms the ability of the vaccine immunogen to do this.”
The priming step would be the first stage of a multi-step vaccine regimen aimed at eliciting many different types of bnAbs, he says.
Play00:0006:52MuteSettingsPIPEnter fullscreen
Promise beyond HIV
The strategy of targeting naïve B cells with specific properties is called “germline-targeting,” as these young B cells display antibodies encoded by unmutated, or “germline” genes. Researchers believe the approach could also be applied to vaccines for other challenging pathogens such as influenza, dengue, Zika, hepatitis C viruses and malaria.
“This is a tremendous achievement for vaccine science as a whole,” says Dennis Burton, Ph.D., professor and chair of the Department of Immunology and Microbiology at Scripps Research, scientific director of the IAVI Neutralizing Antibody Center and director of the NIH Consortium for HIV/AIDS Vaccine Development. “This clinical trial has shown that we can drive immune responses in predictable ways to make new and better vaccines, and not just for HIV. We believe this type of vaccine engineering can be applied more broadly, bringing about a new day in vaccinology.”
The clinical trial, IAVI G001, was sponsored by IAVI and took place at two sites: George Washington University (GWU) in Washington, D.C., and the Fred Hutchinson Cancer Research Center (Fred Hutch) in Seattle, enrolling 48 healthy adult volunteers. Participants received either a placebo or two doses of the vaccine compound, eOD-GT8 60mer, along with an adjuvant developed by the pharmaceutical company GSK. Julie McElrath, M.D., Ph.D., senior vice president and director of Fred Hutch’s Vaccine and Infectious Disease Division, and David Diemert, M.D., professor of medicine at GWU School of Medicine and Health Sciences, were lead investigators at the trial sites.
“This is a landmark study in the HIV vaccine field, demonstrating success in the first step of a pathway to induce broad neutralizing antibodies against HIV-1,” McElrath says. “The novel design of the immunogen, the clinical trial and the molecular B cell analyses provide a roadmap to accelerate further progress toward an HIV vaccine.”
Wide network of collaborators
Funding from the Bill & Melinda Gates Foundation, through the Collaboration for AIDS Vaccine Discovery, supported a wide network of partners conducting complex analyses.
The critical assay used to judge the vaccine candidate, epitope-specific single B cell sorting and B cell receptor (BCR) sequencing, was developed and carried out by teams at the NIH Vaccine Research Center, led by Adrian McDermott, Ph.D. (chief of the Vaccine Immunology Program), Richard Koup, M.D. (deputy director and chief of the Immunology Laboratory and Immunology Section), and research scientist David Leggat, Ph.D.; and at Fred Hutch, led by McElrath and senior staff scientist Kristen Cohen, Ph.D. Study design and data analysis were led by staff scientists Allan deCamp, Ph.D., Greg Finak, Ph.D., and Jimmy Fulp at the Vaccine Immunology Statistical Center at Fred Hutch, with assistance from the Schief lab.
The Scripps Research Institute

