Prolonged high dose use of the hormone drug cyproterone acetate is associated with an increased risk of developing a brain tumour, finds a study of over 250,000 women in France published by The BMJ today.
The higher the dose, and the longer the drug is taken for, the greater the risk of meningioma—a mostly non-cancerous brain tumour arising in the layers of tissue (meninges) that surround and protect the brain and spinal cord. However, the risk declines markedly after stopping treatment.
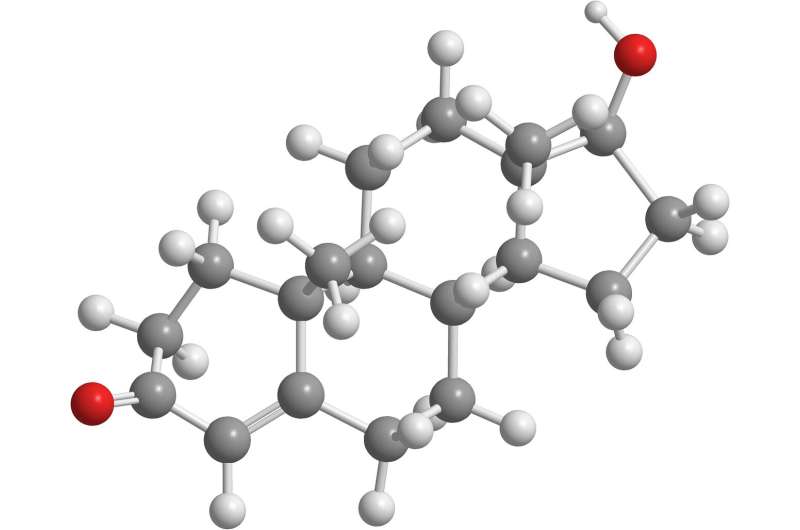
Cyproterone acetate is a synthetic progestogen that lowers testosterone levels. In men it is used to treat inoperable prostate cancer, while in women it is used for conditions such as severe acne and excessive hair growth. Very small doses are also used in birth control pills and hormone replacement therapy.
Since 2007, there have been several reported cases of meningioma associated with prolonged use (5-30 years) of high dose cyproterone acetate (25-100 mg daily) in both men and women. But there is a lack of good quality published evidence on this link.
To address this knowledge gap, researchers set out to evaluate the real life impact of prolonged use of high dose cyproterone acetate (25 or 50 mg/day) on risk of meningioma in girls and women.
The main analysis was based on data for 253,777 girls and women aged 7-70 years (average age 29) living in France who started cyproterone acetate between 2007 and 2014.
All participants had at least one prescription for high dose cyproterone acetate and no history of meningioma, benign brain tumour, or long term disease.
Participants were considered to be exposed when they had received a cumulative dose of at least 3 g during the first six months (139,222 participants) and very slightly exposed (control group) when they had received a cumulative dose of less than 3 g (114,555 participants).
In both groups, treatment was mainly initiated by gynaecologists. Participants were followed up until the end of 2015 and any surgery or radiotherapy for meningioma was recorded.
In the main analysis of women initiating cyproterone acetate, the researchers found 69 meningiomas in the exposed group and 20 meningiomas in the control group treated by surgery or radiotherapy.
This equates to a rate of 23.8 per 100,000 person years in the exposed group and 4.5 per 100,000 person years in the control group.
The majority (60%) of cases were in women over the age of 45 and almost all (96%) underwent invasive surgery. After accounting for other risk factors, such as age and medical history, cyproterone acetate was associated with a 7-fold increased risk of meningioma.
In an additional analysis of 123,997 women already using cyproterone acetate in 2006, the researchers found 463 women with meningioma (a risk of 383 per 100,000 person years in the group with the highest cumulative dose).
However, the risk of meningioma decreased noticeably after treatment was stopped.
This is an observational study, and the researchers point to some limitations that may have affected their results. What’s more, they say this study probably underestimates the overall rate of meningiomas because most small or asymptomatic tumours would not have needed surgery.
Nevertheless, this was a large study based on national prescription data, and the strong dose dependent association, together with the reduction in risk after stopping treatment, suggest a biologically plausible causal relationship.
As such, they say people who use high dose cyproterone acetate for at least three to five years should be informed about the increased risk of meningioma.
Reasons for prescribing cyproterone acetate should also be clearly defined and the lowest possible daily dose used.
When prolonged use of high dose cyproterone acetate is necessary, more thorough screening for meningioma should be considered. And in patients with a documented meningioma, cyproterone acetate should be discontinued, they conclude.
British Medical Journal

